Search results for TCM (34)
New York College & World Found. of TCM

Traditional Chinese Medicine, also known as TCM, includes a range of traditional medicine practices originating in China. Although well accepted in the mainstream of medical care throughout East Asia, it is considered an alternative medical system in much of the Western world. TCM practices include such treatments as Chinese herbal medicine, acupuncture, dietary therapy, and both Tui na and Shiatsu massage. Qigong and Taijiquan are also closely associated with TCM.
Much of the philosophy of traditional Chinese medicine derives from the same philosophy that informs Taoist and Buddhist thought, and reflects the classical Chinese belief that the life and activity of individual human beings have an intimate relationship with the environment on all levels. Read More: > HERE <
New York College of Traditional Chinese Medicine (NYCTCM) by Dr. Chi Chow was started in 1996. Dr. Chow felt that the New York City area had need for a school which taught Traditional Chinese Medicine (TCM) much as it is taught in China, and which at the same time could help students relate this approach to Western medical practice. Her vision included small classes, master-apprentice type teaching relationships in clinic, and the flexibility to accommodate students’ schedules by offering classes mostly on weekends. From its first trimester in Spring of 1996, NYCTCM has embodied this approach.
The mission of the New York College of Traditional Chinese Medicine is to prepare compassionate practitioners who are solidly grounded in the tradition of Chinese medicine, who are able to integrate this tradition within the Western health care system, and who have a spirit of innovation that enables them to adapt a 4000-year-old medicine to 21st-century needs.
NYCTCM Core Values: COMPASSION – In addition to knowledge of TCM theory and mastery of techniques necessary to apply that theory, NYCTCM graduates will bring the emotional qualities of empathy, respect and compassion to all their treatment sessions. TRADITION – NYCTCM graduates will have a thorough understanding of and deep respect for traditional Chinese principles of treatment, including their cultural and philosophical context. INTEGRATION – NYCTCM graduates will have a fundamental understanding of the Western medical approach, and will be able to integrate their practice of TCM within the Western health care system. INNOVATION – NYCTCM graduates will have a spirit of innovation that enables them to adapt a 4000-year-old medicine to 21st-century needs.
The Traditional Chinese Medicine World Foundation is a not-for-profit organization dedicated to educating the public and health-care practitioners about classical traditional Chinese medicine (TCM) and natural self-healing. Through our educational programs, publications, and practitioner resources, we hope to advance the practice and integration of authentic traditional Chinese medicine in Western society.
The TCM World Foundation’s objectives include:* To serve as a source of information on the philosophy, principles, theories, modalities, and practice of authentic TCM and the classical Chinese internal martial arts, such as Qigong and Taiji.* To support the practice of authentic TCM to widen health-care options for the public.* To support an expanded concept of health and healing in contemporary medicine.* To educate individuals on the steps they can take in prevention and self-healing.* To foster a dialogue between Western and Eastern medical schools and communities in the US to improve the quality of training for practitioners of TCM.* To facilitate forums for interdisciplinary collaborations.* To foster balance and harmony in the individual, the community, society, and the world as a whole.
The Foundation’s educational efforts focus on the full system of TCM, which includes: herbal therapy, acupuncture, acupressure, internal martial arts, the prescription of foods for healing, and Chinese psychology. The educational components of the Foundation are geared toward the general public and health-care professionals as well as organizations from both the mainstream and complementary and alternative medicine communities.
Nan Lu, OMD, LAc, is the founding director of the Traditional Chinese Medicine World Foundation and its sister organization, the Tao of Healing. Dr. Lu holds a doctorate from Hubei College of Traditional Chinese Medcine, Hubei, China, and is a New York State-licensed acupuncturist. Classically and university-trained, Dr. Lu is a master herbalist as well as an internationally recognized Taiji expert and Qigong master and the best-selling author of three TCM books published by Harper Collins.
His continuing educational efforts also include the following web sites: www.tcmworld.org, www.tcmconference.org, www.breastcancer.com. http://www.youtube.com/user/masternanlu
Possessing a gift of cross-cultural communication, Dr. Lu lectures internationally and frequently partners with doctors of Western medicine using a preventive and complementary approach. His specialties include women’s health, cancer and immune system disorders and stress management.
Western Herbs from the TCM Perspective
Traditional Chinese Medicine, also known as TCM, includes a range of traditional medicine practices originating in China. Although well accepted in the mainstream of medical care throughout East Asia, it is considered an alternative medical system in much of the Western world.
TCM practices include such treatments as Chinese herbal medicine, acupuncture, dietary therapy, and both Tui na and Shiatsu massage. Qigong and Taijiquan are also closely associated with TCM.
TCM claims to be rooted in meticulous observation of nature, the cosmos, and the human body, and to be thousands of years old. Major theories include those of Yin-yang, the Five Phases, the human body Meridian/Channel system, Zang Fu organ theory, six confirmations, four layers, etc. Read More: > HERE <
Western Herbs from the Traditional Chinese Medicine Perspective
Autor: Ploberger Florian
This book will be published 2011. You can order it now. Traditional Chinese Medicine (TCM) and thus also Chinese phytotherapy is becoming more and more popular. Therefore, so-called Western herbs, which are available to us in the West, are described and therapeutically applied according to TCM criteria. This book describes about 150 herbs such as rosemary, basil, ladys mantle, fumatory, dandelion etc. Besides their English names, pharmaceutical, botanical and German names are also listed for each herb. In addition, a description of the parts of the plants used, their taste, temperature effect, the organs involved and doses is provided as well as detailed descriptions of the actions and individual fields of application of individual herbs.
It is a translation of the 6th revised edition of the book Westliche Kräuter aus Sicht der Traditionellen Chinesischen Medizin.
The book „Westliche Kräuter aus Sicht der Traditionellen Chinesischen Medizin“ (Western Herbs from the Traditional Chinese Medicine Perspective) has been widely published in Europe and its 6th revised edition has already appeared within a few years. It is now being translated into English due to strong demand.
The book: Traditional Chinese Medicine (TCM) and thus also the Chinese phytotherapy is becoming more and more popular. Therefore so-called Western herbs, which are available to us in the West, are described and therapeutically applied according to TCM criteria. This book describes about 150 herbs such as rosemary, basil, ladys mantle, fumatory, dandelion etc. Besides their English names, pharmaceutical, botanical and German names are also listed for each herb. In addition, a description of the parts of the plants used, their taste, temperature effect, the organs involved and doses is provided as well as detailed descriptions of the actions and individual fields of application of individual herbs.
This book serves as an important source of information both for beginners and for experienced therapists.
The author: Dr. med. univ. Florian Ploberger B. Ac., BA Vienna.
Main fields: Traditional Chinese Medicine (TCM) and Tibetan Medicine.
Education: Medical studies and internship in Vienna, study of acupuncture at the Austrian Society of Acupuncture and Auriculotherapy in 1996; three years of TCM studies with Claude Diolosa until 1998; Bachelor in Acupuncture from K.S. University in the USA 1999; four semesters of Sinology studies and numerous study visits to China (TCM University in Beijing, TCM University in Chengdu) and India (LTWA Library of Tibetan Works & Archives). Since 2004 studies of Tibetology at the Vienna University (Bachelor of Arts in the Languages and Cultures of South Asia and Tibet, 2009).
Teaching and publications in the fields of TCM and Tibetan Medicine since 1997.
Head of the Scientific Advisory Council of the Bacopa Centre of Learning in Upper Austria and President of the Austrian Educational Society for Traditional Chinese Medicine (ÖAGTCM) (after three years of further education physicians are awarded the diploma Chinese Diagnostics and Pharmacotherapy by the Austrian Chamber of Physicians).
Regular lectures on Western herbs from the TCM perspective upon invitation of the Austrian Chamber of Pharmacists.
In 2007 he was publishing editor of Die Grundlagen der Tibetischen Medizin (a translation of the book Fundamentals of Tibetan Medicine of Men-Tsee-Khang Publication).
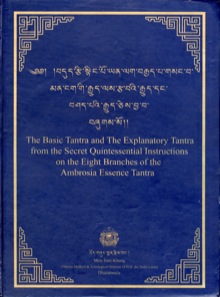
It was a great honour and pleasure for him when in summer 2009 he was officially asked by Dr. Dawa, the Director of the > Men-Tsee-Khang < (Tibetan Medical and Astrology Institute of H.H. the XIVth Dalai Lama in Dharamsala, Northern India) to translate the first two parts of > rGyud-bZhi < , the most important work of Tibetan Medicine (The Basic Tantra and The Explanatory Tantra from the Secret Quintessential Instructions on the Eight Branches of the Ambrosia Essence Tantra).
Since the 12th century this text has been serving as the foundation stone in the training of Tibetan medical practitioners, and is still being learned and memorised today.
Currently, as university reader, he gives a weekly lecture on various subjects of Tibetan Medicine at Vienna University, and every year he spends several months in Dharamsala.
ISBN: 978-3-901618-94-9
The Codex Alimentarius – (Latin for „food code“ or „food book“) is a collection of internationally recognized standards, codes of practice, guidelines and other recommendations relating to foods, food production and food safety. Its name derives from the Codex Alimentarius Austriacus.
Its texts are developed and maintained by the Codex Alimentarius Commission, a body that was established in 1963 by the Food and Agriculture Organization of the United Nations (FAO) and the World Health Organization (WHO).
The Commission’s main aims are stated as being to protect the health of consumers and ensure fair practices in the international food trade. The Codex Alimentarius is recognized by the World Trade Organization as an international reference point for the resolution of disputes concerning food safety and consumer protection. Read More: > HERE <
Herbs in Trad. Chinese Medicine / ChemFoods, and the threat to our freedom of health
Meet NaturalNews.com at facebook <
NaturalNews.com is an independent news resource that covers the natural health and wellness topics that empower individuals to make positive changes in their personal health. NaturalNews offers uncensored news that allows for healthier choice.
WU XING, 5 Elements in TCM, Wu Xing Gong
http://chinese-medicine-works.com/
> TCM – TAI CHI VEREIN SHAMBALA WIEN <
The Wu Xing (Chinese: ä��行; pinyin: wǔxíng), or the Five Movements, Five Phases or Five Steps/Stages, are chiefly an ancient mnemonic device, in many traditional Chinese fields.
It is sometimes translated as Five Elements, but the Wu Xing are chiefly an ancient mnemonic device, hence the preferred translation of „movements“, „phases“ or „steps“ over „elements“. By the same token, Mu is thought of as „Tree“ rather than „Wood“.
The five elements are:
-
* Wood (Chinese: 木, pinyin: mù)
-
* Fire (Chinese: 火, pinyin: huǒ)
-
* Earth (Chinese: 土, pinyin: tǔ)
-
* Metal (Chinese: 金, pinyin: jÄ�n)
-
* Water (Chinese: 水, pinyin: shuǐ)
The system of five phases was used for describing interactions and relationships between phenomena. It was employed as a device in many fields of early Chinese thought, including seemingly disparate fields such as geomancy or Feng shui, astrology, traditional Chinese medicine, music, military strategy, martial arts. Read More: > HERE <
FOUNDATION CONCEPTS OF CHINESE MEDICINE:
Every medicine is a language, a vocabulary of concepts that expresses fundamental beliefs about the nature of reality. It is through this grid that we perceive and explain ourselves. Medical thinking defines human experience, from physiological process to human behavior and competence. It is medicine that determines how we are born and how we die, whether we are fit or disabled, intelligent or ignorant, healthy or ill.
Medicine is the cultural institution that defines when we are alive, valuable, and human. Ontology and pathology are always closely linked: how people get sick is inextricably tied to who they are. The ideas of Chinese medicine differ fundamentally from those of Western medicine, so identifying and solving problems within its context requires familiarity with its concepts, categories, and logic.
Western medicine emerges from the Cartesian model that pictures the world as a machine. Reality is located in what is tangible and material, that which can be measured, quantified, and reduced to smaller and smaller constituent parts. Descartes unequivocally separated mind from body because the existence of consciousness could not be verified by the instruments of science.
Where as modern medicine relies upon the Cartesian–Newtonian reductionist paradigm, Chinese medicine is embedded within the Daoist– Confucianist philosophy of holism. In the Eastern world view, a human being is a living microcosm, a fusion of cosmic and terrestrial forces, the offspring of Heaven and Earth. A person is recognized as a being with a self– aware mind embodied in physical form. The unseen and seen, psyche and soma, are mutually valid and cogenerative: the body provides a home for the mind, and the spirit, nestled securely within the body, animates physical life.
Chinese medical logic postulates that by observing patterns in the external world, the dynamics of human nature are known––as above, so below.
The world is a single, unbroken wholeness–– Dao––that exists without and within. This logic relies upon correspondence thinking: things that correspond to the same thing correspond to each other. Human physiology and identity in Chinese medicine proceed from the assumption that each person is a universe in miniature, so the same forces that shape the macrocosm swirl within each of us, organizing our interior.
Qigong (or ch’i kung) is an internal Chinese meditative practice which often uses slow graceful movements and controlled breathing techniques to promote the circulation of qi within the human body, and enhance a practitioner’s overall health. There are also many forms of qigong that are done with little or no movement at all, in standing, sitting and supine positions; likewise, not all forms of qigong use breath control techniques. Although not a martial art, qigong is often confused with the Chinese martial art of tai chi. This misunderstanding can be attributed to the fact that most Chinese martial arts practitioners will usually also practice some form of qigong and to the uninitiated, these arts may seem to be alike. There are more than 10,000 styles of qigong and 200 million people practicing these methods.
There are three main reasons why people do qigong: 1) To gain strength, improve health or reverse a disease 2) To gain skill working with qi, so as to become a healer 3) To become more connected with the „Tao, God, True Source, Great Spirit“, for a more meaningful connection with nature and the universe. Read More: > Here <
Willkommen auf den Webseiten des tao-chi:
- www.tao-chi.info
- mehr als 300 Seiten Bilder und Texte über unsere Schule für:
- Kung-Fu
- Tai-Chi Ch’uan
- Qi-Gong
- Meditation.
Tierstile sind Bewegungsformen (Formeln), die bereits in prähistorischen Zeiten von Menschen ausgeübt wurden, mit dem Ziel, sich durch Imitation Zugang zu natürlichen Kraftpotentialen zu verschaffen.
Der legendäre Arzt, > Hua-To ( Chinese Physician ) <, (190-265 u.Z.), gilt als Erfinder der “Kunst der fünf Tiere” (Wu Ching Shu), mit der die….“ 5 Elementaren Energien und Kräfte des Inneren gestärkt werden …” sollen und Langlebigkeit erreicht wird. Seine Kunst leitete er aus älteren Traditionen ab, die bis in das 2. Jahrtausend vorchristlicher Zeit zurückreichen.
Pai-Yu Feng war einer der ersten Meister der Shaolin-Schule, der Tierstile im Kung-Fu des Shaolin-Tempels entwickelte und einführte, weshalb sein Name in der Shaolin-Tradition in Ehren gehalten wird.
” Tierstile im Kung-Fu und Qi-Gong “ des Ch’an Shaolim Si Tao“
REFERENCE BOOK: > THE ROOT OF CHINESE QI GONG < : Secrets of Health, Longevity, & Enlightenment: Secrets for Health, Longevity and Enlightenment (Taschenbuch)
“ Qigong befaßt sich mit dem Studium unseres „Energiefeldes“ und hat einen direkten Bezug zu unserer physischen, emotionalen, mentalen und geistigen Gesundheit. Sowohl in den östlichen als auch in den westlichen Geistesschulen sucht man nach Mitteln, um die körperliche Energie positiv zu beeinflussen, entweder indirekt über geistige und emotional wirksame Techniken oder durch direkte Steuerung des Bewusstseins.
In den östlichen Lehrsystemen ist man sich jedoch mehr als im Westen darüber bewusst, welchen Einfluß die Energie (Chi) auf Körper und Geist hat. So arbeitet die TCM (Traditionelle chinesische Medizin) mit Akupunktur und Kräuterheilkunde, mit Moxa und Qigong, um das Chi im inneren zu bewegen und so die Organe zu kräftigen. Im Qigong beginnst Du, ähnlich wie im Yoga mit der körperlichen Übung, bewegst die Energie in Deinen Energiebahnen (Meridiane), bringst Ordnung in Deine Gedanken und erreichst schließlich geistige Klarheit, das Ziel der Meditation.“
Qigong ist demnach der Sammelbegriff für verschiedene Übungsformen, welche ihre Anwendung finden in der Kampfkunst und der Meditation, in der Heilkunst und der Gesundheitspflege. Die Übungen dienen der Stärkung von Körper, Geist und Lebenskraft.
In unserer Tao-Chi Schule für Qi-Gong & Tai-Chi Ch’uan lernen Sie das Qigong-Yangsheng aus dem Lehrsystem von Prof. Jiao Guorui „Das Spiel der 5 Tiere“ (Wu-Chin-Hsi, Wu Xing Gong),Freihandübungen der Shaolin, sowie Handgriffe (Tui-Na, An-Mo) und traditionelle Übungsreihen aus der daoistischen Schule im Rahmen des Tai-Chi Ch’uan-Unterrichtes.
Galangal, TCM, Western Plants in Medicine

> GALGANT , HILDEGARD´s MEDICINE <
> LI SHI ZEN PRIVATUNIVERSITÄT <
> Zingiber off. – Naturheilkunde EU(+Yoga) <
> TCM mit westlichen Pflanzen <
> Kleiner Galgant, Chinesisch 山奈 <
The Galangal plant (Galanga, Blue Ginger) is a rhizome with culinary and medicinal uses. (Lao: ຂ່າ „Kha“; Thai: ข่า „Kha“; Malay: lengkuas (Alpinia galangal); Traditional Mandarin: 南薑 or 高良薑; Simplified Mandarin: 南姜 or 高良姜; Cantonese: lam keong, 藍薑; Vietnamese: Riềng).
It is used in various oriental cuisines (for example in Thai cuisine Tom Yum soups and Dtom Kha Gai, Vietnamese Huenian cuisine (Tre) and throughout Indonesian cuisine, for example, in Soto). Though it is related to and resembles ginger, there is little similarity in taste. Alpinia galanga is also known as Chewing John, Little John Chew and galanga root. It is used in African-American folk medicine. Read More: > Here <
Lesser galangal or Alpinia officinarum (synonym Languas officinarum) is a plant in the ginger family and native to China, growing mainly on the southeast coast. It is also grown in India which is the second largest exporter of the rhizome. The rhizome was widely used in ancient and medieval Europe.
The rhizome is smaller than greater galangal. The skin and the flesh are reddish brown whereas greater galangal has light yellow or white flesh. It was preferred to greater galangal because of its stronger, sweeter taste with notes of cinnamon. Its use in Europe has dramatically declined, however, and is now only used in Eastern Europe. It is used in Russia for flavoring vinegar and the liqueur Nastoika. It is still used as a spice and medicine in Lithuania and Estonia. In Central Asia, Tartars prepare a kind of tea that contains it. The spice used in South Eastern Asia which often goes by the name of „Lesser Galangal“ is actually Kaempferia galanga.
The word lesser galangal properly refers to Alpinia officinarum. In common usage, however, it is also applied to Kaempferia galanga, also called Kencur, Sand ginger, Aromatic Ginger or Resurrection Lily. Kaempferia Galanga, which is grown for medicine and as a spice, is an almost stemless plant that develops its few short-lived leaves and the flower at ground level, whereas the stem of A. officinarum is two to four feet high.
- Meet St. Hildegard friends, studies at facebook <
- Meet Int. Society of Hildegard von Bingen Studies is on fb <
- Meet Islamic Medicine and Studies at fb <
- Meet Ayurveda Friends, Groups, Studies at facebook <
- Meet Traditional Chinese Medicine, studies, friends at fb <
- Meet Tradtional Chinese Medicine I , studies, friends at fb <
- Meet NaturalNews.com , Medicine, Studies, friends, at fb <
NaturalNews.com is an independent news resource that covers the natural health and wellness topics that empower individuals to make positive changes in their personal health. NaturalNews offers uncensored news that allows for healthier choice.
TCM – TRADITIONAL CHINESE MEDICINE
(Traditional Chinese Pulsediagnosis)
> ÖAGTCM: Österr. Ausbildung für TCM <
Traditional Chinese Medicine, also known as TCM, includes a range of traditional medicine practices originating in China. Although well accepted in the mainstream of medical care throughout East Asia, it is considered an alternative medical system in much of the Western world. TCM practices include such treatments as Chinese herbal medicine, acupuncture, dietary therapy, and both Tui na and Shiatsu massage. Qigong and Taijiquan are also closely associated with TCM.
Much of the philosophy of traditional Chinese medicine derives from the same philosophy that informs Taoist and Buddhist thought, and reflects the classical Chinese belief that the life and activity of individual human beings have an intimate relationship with the environment on all levels. Read More: > HERE <
TRADITIONAL CHINESE MEDICINE – Introduction – Traditional Chinese medicine (Simplified: ä��医学; Traditional: ä��醫學; Pinyin: zhōngyÄ� xué) is the name commonly given to a range of traditional medical practices used in China that have developed over the course of several thousand years of history. It is one of the most important forms of Oriental medicine, a term which may also include other related traditional Asian medical systems such as Japanese, Korean, Tibetan, and Mongolian medicine. Chinese medicine principally employs a method of analysis and synthesis, inquiring on a macro-level into the internal systems of the human body and their mutual relationships with the internal and external environment in an attempt to gain an understanding of the fundamental laws which govern the functioning of the human organism, and to apply this understanding to the treatment and prevention of disease, and health maintenance. TCM is rooted in a unique, comprehensive and systematic theoretical structure which includes the Theory of Yin-yang , the Five Elements, the human body Meridian system, and other systems. Treatment is conducted with reference to this philosophical framework.
Uses – In the West, TCM is often considered alternative medicine; however, in mainland China and Taiwan, TCM is widely considered to be an integral part of the health care system. The term TCM is sometimes used specifically within the field of Chinese medicine to refer to the standardized set of theories and practices introduced in the mid-20th century under the government of Mao, as distinguished from related traditional theories and practices preserved by people in Taiwan, Hong Kong and by the overseas Chinese. The more general sense is meant in this section.
TCM developed as a form of noninvasive therapeutic intervention (also described as folk medicine or traditional medicine) rooted in ancient belief systems, including traditional religious concepts. Chinese medical practitioners before the 19th century relied on observation, trial and error, which incorporated certain mystical concepts. Like their Western counterparts, doctors of TCM had a limited understanding of infection, which predated the discovery of bacteria, viruses (germ theory of disease) and an understanding of cellular structures and organic chemistry. Instead they relied mainly on observation and description on the nature of infections for creating remedies. Based on theories formulated through three millennia of observation and practical experience, a system of procedure was formed as to guide a TCM practitioner in courses of treatment and diagnosis.
Unlike other forms of traditional medicine which have largely become extinct, traditional Chinese medicine continues as a distinct branch of modern medical practice, and within China, it is an important part of the public health care system. There are thousands of years of empirical knowledge about TCM conceptualized and recorded in terms appropriate to that system, and in recent decades there has been an effort to integrate the discoveries made by traditional Chinese medicine with the discoveries made by workers in the Western medical traditions. One important component of this work is to use the instrumentation and the methodological tools available via Western medicine to investigate observations made and hypotheses raised by the Chinese tradition.
That this effort has occurred is surprising to many for a number of reasons. In most of the world, indigenous medical practices have been supplanted by practices brought from the West, while in Chinese societies, this has not occurred and shows no sign of occurring. Furthermore, many have found it peculiar that Chinese medicine remains a distinct branch of medicine separate from Western medicine, while the same has not happened with other intellectual fields. There is, for example, no longer a distinct branch of Chinese physics or Chinese biology.
TCM is used by some to treat the side effects of chemotherapy, treating the cravings and withdrawal symptoms of drug addicts and treating a variety of chronic conditions that conventional medicine is claimed to be sometimes ineffective in treating. TCM has also been used to treat antibiotic-resistant infection.
A report issued by the Victorian state government in Australia describes TCM education in China: – Graduates from TCM university courses are able to diagnose in western medical terms, prescribe western pharmaceuticals, and undertake minor surgical procedures. In effect, they practice TCM as a specialty within the broader organization of Chinese health care.
TCM education in Australia, however, does not qualify a TCM practitioner to prescribe scheduled pharmaceuticals, nor to undertake surgical procedures or diagnose in western medical terms.
Theory – There are many schools of thought on which TCM is based. Because of this, the foundation principles of Chinese medicine are not necessarily uniform. Received TCM can be shown to be most influenced by Taoism, Buddhism, and Neo-Confucianism.
For over 3000 years (1200 BCE- present), Chinese academics of various schools have focused on the observable natural laws of the universe and their implications for the practical characterization of humanity’s place in the universe. In the I Ching and other Chinese literary and philosophical classics, they have described some general principles and their applications to health and healing:
- There are observable principles of constant phenomenal change by which the Universe is maintained.
- Man is part of the universe and cannot be separated from the universal process of change.
- As a result of these apparently inescapable primordial principles, the Universe (and every process therein) tends to eventually balance itself.
- Optimum health should result from living as harmoniously as possible with the spontaneous process of change tending towards balance. If there is no change (stagnation), or too much change (catastrophism), balance is increasingly lost and illnesses can occur.
- Everything is ultimately interconnected.
- Always use a systemic approach when addressing imbalances.
TCM is therefore largely based on the philosophical concept that the human body is a small universe with a set of complete and sophisticated interconnected systems. Those systems usually work in balance to maintain the healthy function of the human body. The balance is described as necessarily including qi, blood, jing, bodily fluids, the wu xing, emotions, and spirit (shen). TCM has a unique model of the body, notably concerned with the meridian system. TCM isn’t monolithic, however, and there are from minor to significant regional and philosophical differences between practitioners and schools which in turn can lead to differences in practice and theory.
Macro Views to Diseases – TCM has a macro view to most diseases: well-balanced human bodies can usually handle most everyday bacteria and virus, which are ubiquitous and fastly changing; diseases happens only if there are some unbalanced parts in a human body. Due to this macro philosophy, TCM usually does not care what exact bacteria or virus are causing the symptoms, but tries the best to find which parts of the body are unbalanced as well as to find a strategy to bring back the balance. At the meantime, TCM believes only symptoms matter because irregular symptoms from the human bodies are the only faithful sources to deduce the unbalanced parts in a dynamic, complex system like a human body.
Consequently, the treatments in TCM do not directly target to kill bacteria or virus but to bring back the balance of human bodis. It is very surprising but understandable that a TCM doctor may give very different herb prescriptions to patients affected by a same type of bacteria, because the different symptoms from the patients indicate different unbalanced parts in their bodies.
TCM’s macro view to diseases has some advantages and limitations compared to modern western medicine, which directly targets the external factors of diseases like bacteria and virus.
* The biggest advantage of TCM is that the internal reasons of diseases are addressed and the details of bacteria and virus can be largely ignored. The real potentials of the well-evolved human bodies are used to fight the bacteria and virus instead of simple antibiotics.
A correct TCM treatment will not only address current disease but also establish a strong balance to fight any other diseases. This is especially useful when the abused antibiotics fasten the mutation of bacteria and virus nowadays and it is increasingly difficult for doctors to develop right drugs to kill some specific variants. More over, the downside of western drugs is that they kill not only the bad bacteria and virus but they also severely intervene in the proper functioning of human bodies, which in turn worsen the unbalanced human internal system and make patients more susceptible to other types of bacteria and virus. This is the biggest dilemma in modern western medicine as exemplify by chemotherapy and radiotherapy treatments to cancers.
* A TCM doctor handles many types of diseases from hearts, livers, lungs, etc because the macro view of human body. A patient can be helped by just one visit to a TCM doctor in a comprehensive way. On the other hand, modern western medicine adopts a micro view. The diagnoses and treatments to diseases are highly specialized in terms of different causes. Patients have to judge first which specialist is going to help their problems.
* Judging the effectiveness of treatments in TCM is also based on a macro point of view. Genuine TCM does not rely on micro level lab test results like blood pressure, liver function, a report, bacteria numbers etc. Instead, macro level human feelings and behaviors are used: such as the sleep quality, feeling of enough energy to handle daily work, appetite to food, normal excreting, warmness of hands and feet etc. Modern western medicine relies on the lab tests to see the effectiveness of a treatment using drugs: like how many bacteria are left in the body. TCM doctors often criticize that western doctors pays too much attentions to individual metrics in lab reports and less concerns are given to the overall feelings of patients.
* The cost associated with TCM diagnoses and treatments are usually much less than modern western ways, which requires high-tech equipments and lab facilities to locate the external details. It is relatively fair for both the rich and the poor when seeing a TCM doctor and using Chinese herbs.
* The major problem in TCM is that a right disease diagnosis highly depends on the experiences of a TCM doctor. Even with a right diagnosis, a proper strategy using combined herb prescriptions must be used to bring back the dynamic balance in human bodies. As a result, it takes years or even decades to train a good TCM doctor who can deduce the unbalanced parts from complex symptoms from patients and find a right solution for it considering the interconnection between different parts in human bodies. There is a Chinese saying describing the wisdom and experiences needed for a TCM doctor: A good TCM doctor is also qualified to be a good prime minister in a country. In contrast, modern western diagnoses and treatments are more reliable than TCM in the sense that clear procedures are defined and the accurate information of bacteria and virus can be obtained.
* Finally, TCM may fail if a patient’s internal balance has been ruined too much and immediate, direct solution must be used to fight the diseases. TCM just does not know what bacteria and virus are the culprits.
It is natural for people to think a combined way to fight diseases from both internal and external point of views. Many doctors are researching into this promising areas.
Diagnostics – Following the macro philosophy, TCM diagnostics are based on overall observation of human syptoms rather than micro level labs. There are four types of TCM diagnostic methods: observe (望 wàng), hear and smell (聞 wén), ask about background (問 wèn) and read the pulse (切 qiè). Then a diagnosis is made using a system to classify the symptoms. As mentioned earlier, diagnostic based on symptoms, not bacteria or virus, is the essence in TCM because the internal reasons in human bodies matter.
Systems of diagnosis include:
- * Yin or Yang
- * Five Elements
- * Eight Principles
- * Zang Fu theory
- * Meridian (Chinese medicine)
- * Six Levels
- * Four Stages
- * Three Jiao
TCM diagnosis in China is becoming integrated with western diagnostic thought and is moving towards total integration of the two systems. Modern practitioners in China often use the two systems in combination to understand what is happening with the patient.
Because traditional Chinese medicine predates the more invasive medical testing used in conventional Western medicine, TCM requires skill in a range of diagnostic systems not commonly used outside of TCM. Much of this diagnostic skill involves developing the abilities to observe subtle appearances; to observe that which is right in front of us, but escapes the observation of most people. SEE Also: Traditional Chinese Medicine :: Diagnostic Theory
Diagnostic Techniques
- Palpation of the patient’s radial artery pulse in six positions
- Observation of the appearance of the patient’s tongue
- Observation of the patient’s face
- Palpation of the patient’s body (especially the abdomen) for tenderness
- Observation of the sound of the patient’s voice
- Observation of the surface of the ear
- Observation of the vein on the index finger on small children
- Comparisons of the relative warmth or coolness of different parts of the body
- Anything else that can be observed without instruments and without harming the patient
- SEE Also: Traditional Chinese Medicine :: Diagnostic Theory
Treatment Techniques
- Historically, eight branches comprised Chinese medicine treatment:
- Tui na(推拿) Chinese Massage Therapy
- Acupuncture and Moxibustion(針灸)
- Chinese herbal medicine(ä��药)
- Chinese food therapy食 疗
- Qigong(氣功) and related breathing and meditation exercise
- T’ai Chi Ch’uan (太極拳) and other Chinese martial arts.
- Feng shui风水
- Chinese astrology
Today, all methods except Feng shui and Chinese astrology are routinely used as part of TCM treatments.
Within each treatment branch, specific treatment methods exist. Cupping and Gua sha(刮痧) come under the heading of Tui Na. Auriculotherapy(耳燭療法) comes under the heading of Acupuncture and Moxibustion. Die-da or Tieh Ta (跌打): practitioners who specialize in healing trauma injury such as bone fractures, sprains, bruises etc. Some of these specialists may also use or recommend other disciplines of Chinese medical therapies (or Western medicine in modern times) if serious injury is involved. Such practice of bone-setting is not common in the West.
Modern TCM treatments consist of herbal medicine or acupuncture as the primary method, with other methods such as massage, qi gong, food therapy playing a secondary role. Illness in TCM is seen as a lack of harmony, and the goal of all TCM treatment is to assist the body to regain balance and achieve homeostasis.
The modern practice of traditional Chinese medicine is increasingly incorporating techniques and theories of Western medicine in its praxis.
SEE Also:
- * Health :: Acupuncture
- * Traditional Chinese Medicine :: Moxibustion
- * Traditional Chinese Medicine :: Qigong
- * Traditional Chinese Medicine :: Herbology
- * Traditional Chinese Medicine :: Food Therapy
Traditional Chinese Medicine and Science, The Question of Efficacy – Most scientific research about TCM has focused on acupuncture. Two views have emerged characterized by evidence based medicine on the one hand which has not found convincing evidence for acupuncture and the United States National Institutes of Health on the other, which believed evidence could be uncovered. The 1997 NIH Consensus Statement on Acupuncture summarizes research on the efficacy of acupuncture as follows:
„…promising results have emerged, for example, efficacy of acupuncture in adult post-operative and chemotherapy nausea and vomiting and in postoperative dental pain. There are other situations such as addiction, stroke rehabilitation, headache, menstrual cramps, tennis elbow, fibromyalgia, myofascial pain, osteoarthritis, low back pain, carpal tunnel syndrome, and asthma for which acupuncture may be useful as an adjunct treatment or an acceptable alternative or be included in a comprehensive management program. Further research is likely to uncover additional areas where acupuncture interventions will be useful.“
Much less work in the West has been done on Chinese herbal medicines, which comprise much of TCM. It is clear, however, that some of these medicines have powerful biochemical effects. An example is the herb ephedra which was introduced into the West as a stimulant, and later banned (although this ban was ordered lifted in 2005 by a federal court judge) in the United States after deaths were attributed to its use. A less controversial example is artemisinin, derived from a herb long-used used in TCM, and now used worldwide to treat multi-drug resistant strains of falciparum malaria. In the West, many Chinese medicines have been marketed as herbal supplements and there has been considerable controversy over the regulatory status of these substances.
TCM practitioners usually have no philosophical objections to scientific studies on the effectiveness of treatments. A barrier to the adoption of Chinese herbal medicines into Western practice is finance. It requires a large amount of expertise and money to conduct, for example, a double-blind drug trial, making it a large venture to test even one of the thousands of compounds used by TCM. Because these compounds cannot be patented and owned exclusively, there is a disincentive to sponsor such expensive tests. Some important western medical drugs such as Ephedrine have come from Chinese herbs.
There are also a priori doubts about the efficacy of many TCM treatments that appear to have their basis in magical thinking, e.g. plants with heart-shaped leaves will help the heart, ground bones of tiger give a person energy because tigers are energetic animals and so on.
Purported Mechanism of Action – The basic mechanism of TCM is akin to treating the body as a black box, recording and classifying changes and observations of the patient using a traditional philosophy. In contrast to many alternative and complementary medicines such as homeopathy, practically all techniques of TCM have explanations for why they may be more effective than a placebo, which Western medicine can find plausible. Most doctors of Western medicine would not find implausible claims that qigong preserves health by encouraging relaxation and movement, that acupuncture relieves pain by stimulating the production of neurotransmitters, or that Chinese herbal medicines may contain powerful biochemical agents. However, the largest barriers to describing the mechanisms of TCM in scientific terms are the difference of language and lack of research. TCM concepts such as qi yin and yang are used to describe specific biological processes but are difficult to translate into scientific terms. Some research is now beginning to emerge explaining possible scientific mechanisms behind these TCM concepts.
Safety of Chinese Medicines – Acupressure and acupuncture are largely accepted to be safe from results gained through medical studies. Several cases of pneumothorax, nerve damage and infection have been reported as resulting from acupuncture treatments. These adverse events are extremely rare and were found to be due to practitioner negligence. Dizziness and bruising will sometimes result from acupuncture treatment.
Chinese herbal medicines, in certain cases, involve risk of poisoning or allergic reactions. Cases of acute and chronic poisoning due to treatment through ingested Chinese medicines are relatively common in China, Hong Kong, and Taiwan, with numerous deaths occurring each year. Many of these deaths do occur however, when patients self prescribe herbs or take unprocessed versions of toxic herbs. For example, the Chinese herb má huáng — known commonly in the west by its Latin name Ephedra — was banned in 2004 by the FDA, although, the FDA’s final ruling exempted traditional Asian preparations of Ephedra from the ban. The Ephedra ban was meant to combat the use of this herb in western weight loss products, a usage that directly conflicts with traditional Asian uses of the herb. There were no cases of Ephedra based fatalities with patients using traditional Asian preparations of the herb for its traditionally intended uses. This ban was ordered lifted in April 2005 by a Utah federal court judge.
Furthermore, potentially toxic and carcinogenic compounds such as arsenic and cinnabar are sometimes prescribed as part of a medicinal mixture or used on the basis of „using poison to cure poison“. Unprocessed herbals are sometimes adulterated with chemicals that may alter the intended effect of a herbal preparation or prescription. Much of these are being prevented with more empirical studies of Chinese herbals and tighter regulation regarding the growing, processing, and prescription of various herbals.
Traditional Chinese Medicine and Western Medicine – Within China, there has been a great deal of cooperation between TCM practitioners and Western medicine, especially in the field of ethnomedicine. Chinese herbal medicine includes many compounds which are unused by Western medicine, and there is great interest in those compounds as well as the theories which TCM practitioners use to determine which compound to prescribe. For their part, advanced TCM practitioners in China are interested in statistical and experimental techniques which can better distinguish medicines that work from those that do not. One result of this collaboration has been the creation of peer reviewed scientific journals and medical databases on traditional Chinese medicine.
The relationship between TCM and Western medicine in the West is more contentious. While more and more medical schools are including classes on alternative medicine in their curricula, older Western doctors and scientists are far more likely than their Chinese counterparts to skeptically view TCM as archaic pseudoscience and superstition. This skepticism can come from a number of sources. For one, TCM in the West tends to be advocated either by Chinese immigrants or by those that have lost faith in conventional medicine. Many people in the West have a stereotype of the East as mystical and unscientific, which attracts those in the West who have lost hope in science and repels those who believe in scientific explanations. There have also been experiences in the West with unscrupulous or well-meaning but improperly-trained „TCM practitioners“ who have done people more harm than good in many instances.
As an example of the different roles of TCM in China and the West, a person with a broken bone in the West (i.e. a routine, „straightforward“ condition) would almost never see a Chinese medicine practitioner or visit a martial arts school to get the bone set, whereas this is routine in China. As another example, most TCM hospitals in China have electron microscopes and many TCM practitioners know how to use one.
This is not to say that TCM techniques are considered worthless in the West. In fact, Western pharmaceutical companies have recognized the value of traditional medicines and are employing teams of scientists in many parts of the world to gather knowledge from traditional healers and medical practitioners. After all, the active ingredients of most modern medicines were discovered in plants or animals. The particular contribution of Western medicine is that it strictly applies the scientific method to promising traditional treatments, separating those that work from those that do not. As another example, most Western hospitals and increasing numbers of other clinics now offer T’ai Chi Ch’uan or qigong classes as part of their inpatient and community health programs.
Most Chinese in China do not see traditional Chinese medicine and Western medicine as being in conflict. In cases of emergency and crisis situations, there is generally no reluctance in using conventional Western medicine. At the same time, belief in Chinese medicine remains strong in the area of maintaining health. To put it simply, you see a Western doctor if you have acute appendicitis, but you do exercises or take Chinese herbs to keep your body healthy enough to prevent appendicitis, or to recover more quickly from the surgery. Very few practitioners of Western medicine in China reject traditional Chinese medicine, and most doctors in China will use some elements of Chinese medicine in their own practice.
A degree of integration between Chinese and Western medicine also exists in China. For instance, at the Shanghai cancer hospital, a patient may be seen by a multidisciplinary team and be treated concurrently with radiation surgery, Western drugs and a traditional herbal formula.
It is worth noting that the practice of Western medicine in China is somewhat different from that in the West. In contrast to the West, there are relatively few allied health professionals to perform routine medical procedures or to undertake procedures such as massage or physical therapy.
In addition, Chinese practitioners of Western medicine have been less impacted by trends in the West that encourage patient empowerment, to see the patient as an individual rather than a collection of parts, and to do nothing when medically appropriate. Chinese practitioners of Western medicine have been widely criticized for overprescribing drugs such as corticosteroids or antibiotics for common viral infections. It is likely that these medicines, which are generally known to be useless against viral infections, would provide less relief to the patient than traditional Chinese herbal remedies.
Traditional Chinese Medicine and Animals – As animal products are used in Chinese formulas, vegans and vegetarians should inform their practitioner, if their beliefs forbid the ingestion of animals. Often alternative substances can be used.
The use of endangered species is controversial within TCM. In particular, the belief that tiger penis and rhinoceros horn are aphrodisiacs has been blamed for depleting these species in the wild. Medicinal use is also having a major impact on the populations of sea horses.
The animal rights movement notes that a few traditional Chinese medicinal solutions use bear bile. To extract maximum amounts of the bile, the bears are often fitted with a sort of permanent catheter. The treatment itself and especially the extraction of the bile is very painful, causes damage to the intestines of the bear, and often even kills the bears. However, due to international attention on the issues surrounding its harvesting, bile is now rarely used by practitioners outside of China.
- Sources
- * Chang, Stephen T. The Great Tao; Tao Longevity; ISBN 0942196015 Stephen T. Chang
- * Kaptchuck, Ted J., The Web That Has No Weaver; Congdon & Weed; ISBN 0809229331Z
- * Maciocia, Giovanni, The Foundations of Chinese Medicine: A Comprehensive Text for Acupuncturists and Herbalists; Churchill Livingstone; ISBN 0443-039801
- * Ni, Mao-Shing, The Yellow Emperor’s Classic of Medicine : A New Translation of the Neijing Suwen with Commentary; Shambhala, 1995; ISBN 1570620806
- * Holland, Alex Voices of Qi: An Introductory Guide to Traditional Chinese Medicine; North Atlantic Books, 2000; ISBN 1556433263
- * Unschuld, Paul U., Medicine in China: A History of Ideas; University of California Press, 1985; ISBN 0520050231
- * Qu, Jiecheng, When Chinese Medicine Meets Western Medicine – History and Ideas (in Chinese); Joint Publishing (H.K.), 2004; ISBN 9620423364
- * Chan, T.Y. (2002). Incidence of herb-induced aconitine poisoning in Hong Kong: impact of publicity measures to promote awareness among the herbalists and the public. Drug Saf. 25:823–828.
- * Benowitz, Neal L. (2000) Review of adverse reaction reports involving ephedrine-containing herbal products. Submitted to U.S. Food and Drug Administration. Jan. 17.
- * Porkert, Manfred The Theoretical Foundations of Chinese Medicine MIT Press, 1974 ISBN 0262160587
- * Hongyi, L., Hua, T., Jiming, H., Lianxin, C., Nai, L., Weiya, X., Wentao, M. (2003) Perivascular Space: Possible anatomical substrate for the meridian. Journal of Complimentary and Alternative Medicine. 9:6 (2003) pp851-859
Links
- State Administration of Traditional Chinese Medicine for the People’s Republic of China, (English)
- Journal of Chinese Medicine
- Classics of Traditional Chinese Medicine, by the National Library of Medicine (NLM)
- Merging Chinese Traditional Medicine into the American Health System
- The Chinese Medicine Sampler- Historical Roots of Traditional Chinese Medicine
- An essay on translation of Chinese concepts into English
- Traditional Chinese Medicine news, information, education, research and discussion – A regularly updated TCM website based in Australia
- ChineseMedicine.com.hk 香港ä��醫網
- National Certification Commission for Acupuncture and Oriental Medicine (USA)
- University Minnesota – What is TCM ?
- AHC – Center for Spirituality and Healing
- QI GONG im Kloster St. Clemens, July 2010
- Guang’anmen HOSPITAL, CHINA ACADEMY of Chinese Medical Sciences
- Meet QI-GONG Groups and Friends at facebook <
TCM, TRAD. AYURVEDA AND PULSDIAGNOSES
Introduction to Buddhist Ayurveda or Tibetan Medicine – Vata Dosha (Space and Air), Pitta Dosha (Fire and Water), Kapha Dosha (Water and Earth) — Lectures from the „Four Tibetan Medical Tantras“ („rGyud – bzhi“ in Tibetan, pronounced „Ju Shee“ — „Si-Bu-Yi-Dian in Mandarin — in Sanskrit it is called the „Amrta-hrdaya-astanga-guhyopadesa-tantra“ or Amrita Hridaya Astanga Guhyopadesha Tantra)
- >* VIDEO INTRO TO BUDDHIST AYURVEDA OR TIBETAN MEDICINE * <
- >* VIDEO Ayurveda Arthritis Chinese Medicine, Rheumatism …* <
Nalanda College of Buddhist Ayurveda of Nalanda University, part of the 501(c)3 Non-Profit Religious Organization Medicine Buddha Wholistic Ministry – Anonymous American Buddhist Monk of Geluk Nalanda Tradition of Tibet and India, Ayur-Vedic Herbal Medicine Practitioner (http://www.Ayurveda-Berkeley.com – 510-292-6696 in Berkeley, California)AYR220 Ayurvedic Consultation 001 Constitutional Medicine Tibetan Medicine Ayurveda Intake-Form (October 26, 2008)
Dr. Florian Ploberger, Wien , Lehrtätigkeit und Publikationen in den Themenbereichen TCM und Tibetische Medizin seit 2000 im Bacopa Bildungszentrum. Leiter des Wissenschaftlichen Beirates des Bacopa-Bildungszentrum in Oberösterreich sowie Präsident der Österreichischen Ausbildungsgesellschaft für Traditionelle Chinesische Medizin (ÖAGTCM).
BUCHTIPP: > Wurzel-Tantra & Tantra der Erklärungen des rGyud-bZhi , die vier Tantras der Medizin < (The Basic Tantra and The Explanatory Tantra from the Secret Quintessential Instructions on the Eight Branches of the Ambrosia Essence Tantra.) Dieser Text dient seit dem 12. Jahrhundert als Grundlagentext in der Ausbildung der tibetischen Mediziner und wird noch heutzutage auswendig gelernt.
2007 wurde er an den Men-Tsee-Khang (Schule für tibetische Medizin und Astrologie unter der Schirmherrschaft des XIV. Dalai Lama in Dharamsala, Nordindien) eingeladen, um dort Vorträge zu halten.
Zurzeit hält er wöchentlich an der Universität Wien eine Vorlesung über diverse Themen der Tibetischen Medizin und verbringt jedes Jahr mehrere Monate in Dharamsala.
Zu seiner grossen Freude und Ehre wurde er im Sommer 2009 offiziell von Dr. Dawa, dem Direktor des Men-Tsee-Khang, mit der Übersetzung der ersten beiden Teile des bedeutendsten Werkes der tibetischen Medizin: ( rGyud-bZhi*. Deutscher Titel: Vier Tantra der Medizin) beauftragt.
> Pulsdiagnose, die sanfte Botschaft des Körpers <
In diesem Buch werden tiefe Einblicke in die Kunst der Pulsdiagnostik gewährt. Die Autoren beschreiben die Pulsdiagnostik aus Sicht zweier verschiedener traditioneller, östlicher Medizinsysteme: der ayurvedischen und chinesischen Medizin.
Für eine korrekte Diagnostik ist die Pulstastung von entscheidender Bedeutung. In diesem praxisorientierten Buch werden alle wichtigen Aspekte des Pulses unter dem Blickwinkel der verschiedenen Krankheitsmuster dargestellt. Es vermittelt die Technik der Pulstastung sowie die klinische Bedeutung der klassischen Pulsqualitäten.
Die Vorteile für Sie:
- Pulsdiagnostik in 2 verschiedenen Medizinsystemen
- Starker Bezug zur Praxis
- Graphische Darstellung aller Pulsqualitäten
-
Dieses Buch dient sowohl Einsteigern als auch erfahrenen Therapeuten als wichtige Informationsquelle.
Die Autoren dieses interkulturellen Werkes sind:
- Frau Dr. Vinod Verma arbeitet und lehrt als Ayurvedischen Ärztin in Europa und Indien.
- Dr. Florian Ploberger ist Arzt für Allgemeinmedizin und Traditionelle Chinesische Medizin in Österreich.
Check out the new @IISD_ELP e-book by Stefanie Schacherer
Opinion: After Jamal Khashoggi’s death we need to re-assess diplomatic immunity https://t.co/s5LO1h8zEH
— Opinio Juris (@opiniojuris) 26. Oktober 2018
Demonstration for academic freedom & @ceuhungary #Hungary. Will government sign the agreement and let CEU continue its important work? 1000s of students, alumni & concerned Hungarians demand it! @ManfredWeber @EPP @EPPGroup pic.twitter.com/91R1rxE8os
— Lydia Gall (@LydsG) 26. Oktober 2018
Authoritarian sensibilities will never be satisfied: „First they came for Népszabadság, then for CEU and NGOs, soon after HírTV too.. now they can’t even tolerate the Academy of Sciences or Corvinus“
– @MomentumHu’s Dániel Berg at #istandwithCEU protest: https://t.co/F2H2miJDPX
— Joost (@almodozo) 26. Oktober 2018
Good morning #London
Super excited about @BIICL conference on investment arbitration & human rights!
Thank you @CALR_UWEBristol and @uwelaw for making this possible! pic.twitter.com/1lf8YqZRhh— Amy Man (@_Amy_Man) 26. Oktober 2018
ICYMI – Seven Reasons Why Feminists Say No to World Bank-IMF Neoliberalism from @apwld https://t.co/JENfddFyHQ pic.twitter.com/n2EvbMvhY7
— GAD Network (@GAD_Network) 26. Oktober 2018
Sir Christopher Greenwood, GBE, CMG, QC keynote address @BIICL #ITF: #Investment should no longer be viewed as self-contained but rather viewed in international #law context pic.twitter.com/edWdmMpWjk
— Amy Man (@_Amy_Man) 26. Oktober 2018
@UN_Vienna in classrooms: Students from the Polytechnical School in #Waidhofen an der Thaya came together to learn more about the #UN and #GlobalGoals and to celebrate #UN Day. pic.twitter.com/aCD2aUJN26
— UN Vienna (@UN_Vienna) 25. Oktober 2018
#CEU announced that the Hungarian government had informed the US ambassador 3 weeks ago: it is not willing to sign the agreement w NY state which would enable the university to stay in #Hungary. @JosephDaul @ManfredWeber @epp #academicfreedom
— Katalin Halmai (@eublogo) 25. Oktober 2018
#ceu Rektor rechtfertigt Ultimatum an Orbán-Regierung mit d.Worten: genug ist genug! CEU lässt sich nicht weiter hinhalten
— Ernst Gelegs (@Gelegs) 25. Oktober 2018
Apparently @ceuhungary will have to move to Vienna in a month — unless Orbán miraculously changes its mind and signs deal with State of NY. Not likely after telling US Amb Cornstein he won’t do that. https://t.co/7thyNLfHLC
— Márta Pardavi (@martapardavi) 25. Oktober 2018
It’s the anniversary of the 1956 Hungarian Uprising, soon brutally crushed by Soviet tanks enforcing Moscow’s Communist Empire.
Some 200,000 Hungarian refugees were welcomed in the West.
Hungary’s ruling party today remembers nothing & runs hate campaigns against refugees. pic.twitter.com/squSyujaOk
— Andrew Stroehlein (@astroehlein) 24. Oktober 2018
The third, concluding panel of this year’s #LegalAdvisersMeeting @UN
focusing on #Memoranda of #Understanding in the light of the #ViennaConvention on the Law of the Treaties inaugurated. Looking forward to an interesting discussion!#TreatyLaw #MoUs #InternationalLawWeek
🇵🇱🇺🇳 pic.twitter.com/Baauq23cIJ— Poland in the UN (@PLinUN) 23. Oktober 2018
The Inter-American Court’s Advisory Opinion on #Asylum and Its Impact for the Human Rights of #Refugees Worldwide https://t.co/HBQfpqqFoD via @opiniojuris #humanrights
— Pace Law Library (@pacelawlibrary) 25. Oktober 2018
Greece says EEZ will be delimitated according to international law (and not based on Turkey’s views) – https://t.co/HCoP3rHLyy
— Opinio Juris (@opiniojuris) 25. Oktober 2018
Imprisoned Ukrainian Director Oleh Sentsov Wins #SakharovPrize . Meanwhile, the 2012 co-winner of Sakharov Prize For Freedom of Thought, Iranian lawyer Nasrin Sotoudeh is also serving a 5 year- prison term.
— Golnaz Esfandiari (@GEsfandiari) 25. Oktober 2018
„Two Authorities, One Way, Zero Dissent: Arbitrary Arrests & Torture by the #Palestinian Authority & Hamas“
If you missed it the first time around, here’s @HRW’s report released earlier this week, https://t.co/JYQKXxveUM pic.twitter.com/zN21dgiwzf
— Lotte Leicht (@LotteLeicht1) 25. Oktober 2018
In #Russia domestic violence puts lives at risk.
Urgently needed: a domestic violence law, protection orders, better access for survivors to shelters.
New @HRW report: ‘I Could Kill You and No One Would Stop Me’https://t.co/8kRwQhgadB pic.twitter.com/nk6phgb76z
— Lotte Leicht (@LotteLeicht1) 25. Oktober 2018
CEU set to leave Hungary: Possibly the most dramatic moment of the day was when a university official said that the move to Vienna of thousands of students, staff, and their families would be the biggest forced exodus from Hungary since 1956. https://t.co/zGu8SeZ37T
— Lili Bayer (@liliebayer) 25. Oktober 2018
More on #PPPs and the problems they carry in terms of transparency, economic risks & sustainable development. „El rol del sector privado en el desarrollo de infraestructura“ (In Spanish) https://t.co/c8IYQNeLVE @eurodad @CoalicionReg
— Bretton Woods Proj. (@brettonwoodspr) 25. Oktober 2018
Interested in analysis of #ISDS decisions having sustainable development implications?
Check out the new @IISD_ELP e-book „International Investment Law & Sustainable Development,“ by Stefanie Schacherer, launched at @UNCTADwif #WIF2018.
Read it here: https://t.co/00WmtJIvdh pic.twitter.com/tCm3uJZQ1i
— Martin D. Brauch (@mdbrauch) 25. Oktober 2018
Myanmar: 7 Years for Reporting the Truth
“It is simply not credible for the British government to claim it supports justice and accountability and then refuse to support referring Burma to the International Criminal Court, which was specifically set up for cases like this.” @MarkFarmaner https://t.co/q2NgyMZEt4
— Burma Campaign UK (@burmacampaignuk) 4. September 2018
Happening NOW- Burma issue discussed in the UK Parliament Foreign Affairs debate- Foreign Secretary @Jeremy_Hunt refuses to support referral of Burma to the International Criminal Court https://t.co/2kphr3rxIy
— Burma Campaign UK (@burmacampaignuk) 4. September 2018
“I urge #Myanmar to immediately & unconditionally release Kyaw Soe Oo and Thet Oo Maung. Their conviction sends a message to all journalists in Myanmar that they cannot operate fearlessly“ — @UNHumanRights Chief Michelle Bachelet: https://t.co/hcy7ZTQCRL #FreeWaLoneKyawSoeOo pic.twitter.com/wBxWfuPDVf
— UN Human Rights (@UNHumanRights) 3. September 2018
SG @antonioguterres urges review of sentence against 2 journalists in Myanmar: https://t.co/ODuqzX2YWP
— UN Spokesperson (@UN_Spokesperson) 3. September 2018
This is difficult to watch. Chit Su and Pan Ei Mon appeal on behalf of their husbands, @Reuters journalists jailed in Myanmar. „I’m very much proud of him. I will also teach my daughter to be proud of her father.“ #FreeWaLoneKyawSoeOo https://t.co/5XVn4Xt0T2 pic.twitter.com/gZRh2Du6sS
— Poppy McPherson (@poppymcp) 4. September 2018
The road to democracy cannot be built on acts of genocide and a road that is should and must only lead to one place, a trial at the International Criminal Court. – Writes @Imran_HussainMP https://t.co/n2tCv7QNKB
— Burma Campaign UK (@burmacampaignuk) 4. September 2018
Today we ask our supporters to write to Wa Lone and Kyaw Soe Oo directly at the prison they are jailed in, to show that people all over the world do care about them, support them and stand by them. Please TAKE ACTION here https://t.co/BFZZoOiibX
— Burma Campaign UK (@burmacampaignuk) 4. September 2018
Powerful statement:
83 #Myanmar groups „strongly condemn“ the verdicts against two @Reuters journalists „for simply doing their jobs“, and call for their „immediately and unconditionally release“#FreeWaLoneKyawSoeOo https://t.co/CsVOMx8AUX pic.twitter.com/pDoRglwYgL
— Lotte Leicht (@LotteLeicht1) 4. September 2018
„We arrived at a position we had not expected … None of us thought the evidence for #genocide would be as strong as it was. That came as a surprise.“ #UN investigator Christopher Sidoti on documenting & analyzing #Myanmar army atrocity crimes. https://t.co/5eIfUFF0sk
— Lotte Leicht (@LotteLeicht1) 3. September 2018
New call for brand support ahead of Bangladesh wage talks | Apparel Industry News | just-style https://t.co/b7X9pBii23 via @juststyle
— Labor Rights Forum (@ILRF) 29. August 2018
„Unwilling to upset our great ally and protege Aung San Suu Kyi, we resisted calls for an independent investigation into war crimes. Instead, we encouraged the Myanmar leader to carry out her own investigation.“ Writes Peter Oborne@OborneTweets https://t.co/a9VVEz70mj
— Burma Campaign UK (@burmacampaignuk) 3. September 2018
Today, our Reuters colleagues Wa Lone and Kyaw Soe Oo were sentenced to seven years in jail for exposing a massacre by the Myanmar military. This cartoon in @TheMyanmarTimes sums up the chilling impact the verdict has had on the country’s journalists. #FreeWaLoneKyawSoeOo pic.twitter.com/v1GmpJSc4o
— Andrew RC Marshall (@Journotopia) 3. September 2018
ျမန္မာကုိ ICC ပုိ႔ေရး ၿဗိတိန္အဖြဲ႔ ေတာင္းဆုိ https://t.co/fWk0PQtdJi
— Burma Campaign UK (@burmacampaignuk) 3. September 2018
The NLD-led government has the power to immediately order the release of Wa Lone and Kyaw Soe Oo. The only thing keeping them in jail is Aung San Suu Kyi’s lack of respect for human rights. – Our Executive Director, Anna Roberts @anna_c_roberts https://t.co/vJAICgkTcM
— Burma Campaign UK (@burmacampaignuk) 3. September 2018
Burma Campaign UK today condemned the sentencing of Wa Lone and Kyaw Soe Oo, and urged Aung San Suu Kyi to release them today, and to repeal all repressive laws, which are being used to keep journalists, human rights activists and others in jail for pol… https://t.co/vJAICgkTcM
— Burma Campaign UK (@burmacampaignuk) 3. September 2018
The Official Secrets Act was introduced in 1923, during the colonial era, and carries a maximum prison sentence of 14 years. The government has used the law against journalists in the past to prevent open reporting on government and military activities.
“The attempt by the military to cover up acts of genocide and the decision of the NLD-led government to support this and allow the prosecution to continue highlights many serious problems in Burma today,“ said Anna Roberts, Executive Director at Burma Campaign UK. “There is a climate of growing restrictions on media freedom, and Aung San Suu Kyi must now start facing international pressure over her decision to keep so many repressive laws in place and keep political prisoners in jail.”
Burma Campaign UK is also calling on the European Union to suspend its MyPol training programme with the military-controlled police force, which framed and arrested Wa Lone and Kyaw Soe Oo. As long as the police force is not accountable to the government and under the control of a military accused of genocide, it is hard to see how this can be an effective use of European taxpayers’ money.
Journalism is not a crime pic.twitter.com/c7fY6MkmpL
— Jonathan Landay (@JonathanLanday) 3. September 2018
Thank you Sweden for supporting the referral of Burma to the #ICC. Other UNSC members must now follow and support UN FFM’s recommendations. UK @10DowningStreet must stop protecting Burmese military. https://t.co/gwNksQJQYk
— Burma Campaign UK (@burmacampaignuk) 29. August 2018
Today’s verdict „undermines freedom of the media, the public’s right to information & the development of the rule of law in #Myanmar„#EU decries sentencing of @Reuters journalist Wa Lone & Kyaw Soe Oo, & calls for their immediate & unconditional release https://t.co/tw5k4JLnmO pic.twitter.com/ULOeTFRF5t
— Lotte Leicht (@LotteLeicht1) 3. September 2018
Myanmar Rohingya: How a ‚genocide‘ was investigated – https://t.co/QcZYMoyYov
— Opinio Juris (@opiniojuris) 3. September 2018
As the judge spoke, several reporters cried as they took notes.Kyaw Soe Oo’s wife, Chit Su Win, burst into tears after the verdict, and family members had to support her as she left the court. #FreeWaLoneKwaySoeOo https://t.co/7cchuaBExB
— Parisa Hafezi (@PHREUTERS) 3. September 2018
A dark day for free press in #Myanmar.
Today, a court sentenced two brave @Reuters journalists to 7 years prison.
Their crime? Doing their job and exposing this gruesome massacre.
Meanwhile, impunity for army atrocities continues#FreeWaLoneKyawSoeOo https://t.co/qVX8huxaHM
— Lotte Leicht (@LotteLeicht1) 3. September 2018
On the Intl Day for the Victims of Enforced Disappearance, WUC Project Coordinator Ryan Barry spoke to @AJEnglish about #China’s systematic use of enforced disappearance against #Uyghur & the over 1 million Uyghurs who effectively disappeared into political indoctrination camps. pic.twitter.com/OdzklxUQiz
— WorldUyghurCongress (@UyghurCongress) 1. September 2018
They are at it again, the 8-digit SE Asian bots. Blocking dozens every day. @TwitterSupport @Twitter pic.twitter.com/zUhVEP7gcP
— LaetitiavandenAssum (@lvandenassum) 3. September 2018
US urges Indian Ocean Region countries to reaffirm commitment to global rules and norms – https://t.co/fhT2WJhnUW
— Opinio Juris (@opiniojuris) 3. September 2018
Myanmar’s president, Win Myint, was an MP four years ago. Back then, he had some harsh words on the govt’s use of the Official Secrets Act to prosecute reporters. Today, a court used the same law to lock up two @Reuters journalists for seven years. What will he say now? pic.twitter.com/AxbYuZhrCd
— Timothy McLaughlin (@TMclaughlin3) 3. September 2018
An outrageous injustice. @Reuters journalists, Wa Lone & Kyaw Soe Oo, get 7 years prison for their investigative reporting. #AungSanSuuKyi, is this your #Myanmar? You used to believe in freedom of the press.
Quash the verdicts & #FreeWaLoneKyawSoeOo https://t.co/9tIojzaaGc
— Lotte Leicht (@LotteLeicht1) 3. September 2018
Israeli 19-year-old jailed for refusing military service
Irony of the day: Jared Kushner says NK Leader is unqualified for the job and only got it through nepotism 😉 https://t.co/vJz8cCmTgg
— Toby Cadman (@tobycadman) 12. August 2017
‚Eyes wide shut to suffering.‘
A powerful editorial. The refugees on Manus and Nauru must be brought here. Read why. https://t.co/8XTcMmi8j5— Julian McMahon (@jmcmahonlawyer) 13. August 2017
Former int’l prosecutor & #Syria investigator del Ponte says there’s enough evidence to convict #Assad of war crimes https://t.co/1QAr7BSu1y pic.twitter.com/lTArk7l4a9
— Lotte Leicht (@LotteLeicht1) 13. August 2017
Patrick Kroker @ECCHRBerlin erklärt, wie syrische Kriegsverbrecher trotz Blockade der #UN bestraft werden können. https://t.co/JLfxP18toX
— WELT-SICHTEN (@weltsichten) 9. August 2017
Remember these adorable girls?
Find out how they got on in Canada 🇨🇦 pic.twitter.com/SW79p2C77M— UN Refugee Agency (@Refugees) 13. August 2017
In 2015, cousins Maryam + Sundos were ready to resettle in #Canada. 🇨🇦
Soak up their cuteness, we’ll have a update on their reunion soon! pic.twitter.com/RXfQdUUYJa— UN Refugee Agency (@Refugees) 9. August 2017
“If you’re not outraged, you’re not paying attention.” Last FB post of Heather Heyer, killed in #Charlottesville https://t.co/hqjjCi5MYa pic.twitter.com/7jmJDVU3Lw
— Andrew Stroehlein (@astroehlein) 13. August 2017
“Heather was not about hate, Heather was about stopping hatred. Heather was about bringing an end to injustice.“https://t.co/DqMRcSPXOp
— Lotte Leicht (@LotteLeicht1) 13. August 2017
Hindrance of humanitarian assistance will create a deadly gap in the #Mediterranean Sea, @MSF warns.https://t.co/0hq0QBn8CT
— Lotte Leicht (@LotteLeicht1) 13. August 2017
We are devastated by the death of 7 White Helmets in #Syria. Aid workers are #NotATarget. Sign the petition at https://t.co/kEKc8PyFfc. pic.twitter.com/NkCyN71mI1
— UNOCHA (@UNOCHA) 13. August 2017
S Korean court again orders Japanese (Mitsubishi) firm to compensate WWII forced labor victims https://t.co/sNwonN3VxT
— Opinio Juris (@opiniojuris) 13. August 2017
Share your ideas on National Plan of Actions on the Improvement of the Status of Children in #Belarus till 7 August: https://t.co/jo9JO4YQTw pic.twitter.com/r9FT6cig9m
— UNICEF Belarus (@UNICEF_BY) 1. August 2017
„No one is born hating another person because of the color of his skin or his background or his religion…“ pic.twitter.com/InZ58zkoAm
— Barack Obama (@BarackObama) 13. August 2017
#Egypt: @ShawkanZeid is again at court today. He is on trial with 738 other defendants. This a travesty of justice. #FreeShawkan now! pic.twitter.com/Vub40bgyzY
— EBOHR (@EBOHumanRights) 12. August 2017
68 years later and the #GenevaConventions still matter. pic.twitter.com/7ZW6voj1VZ
— ICRC (@ICRC) 12. August 2017
Int’l attention seems to be fading, but in #Syria war crimes & govt killings of civilians continue w/ utter impunity https://t.co/ggd1pgDURj
— Lotte Leicht (@LotteLeicht1) 12. August 2017
Terrible news from #Syria: seven #WhiteHelmets assassinated in Idlib & equipment stolen. https://t.co/JDaBkeLoEf
— Lotte Leicht (@LotteLeicht1) 12. August 2017
9 people killed in a single family. They were btw 3 and 80 years old.
The devastating cost of #Yemen’s war:@ICRC https://t.co/jhzvzJBEKu— Lotte Leicht (@LotteLeicht1) 12. August 2017
#Schröder is the most prominent German lobbyist for Russian gas and energy policy. But there are more, e.g. Matthias Warnig https://t.co/Uo8IuaiK4K
— Birgit Schmeitzner (@BSchmeitzner) 12. August 2017
Berlin ist groß, die Auswahl an Kneipen auch. Wer sich aufregt, dass Kellner Englisch sprechen, möge einfach nebenan einkehren. #Kleingeist
— Birgit Schmeitzner (@BSchmeitzner) 13. August 2017
„When they step into the stadium, they don’t feel like #refugees any more“ #TeamRefugees at @London2017 @BBCSport https://t.co/gYAyiXZqx7
— Lotte Leicht (@LotteLeicht1) 12. August 2017
To promote the right to play & sport #foreverychild, @UNICEF_BY joined @milanjuniorcamp in #Minsk. Show your support and be active! pic.twitter.com/OknhRcYvKI
— UNICEF Belarus (@UNICEF_BY) 25. Juli 2017
Congratulations again. Sushen Ray of Bengal Police for winning another Gold Medal at World Police Games in LA,USA.This one for triple jump
— Mamata Banerjee (@MamataOfficial) 12. August 2017
Honored to take part in a Forum on #Myanmar Democratic transition @myanmar_moi https://t.co/9nyZ2jlIdw… pic.twitter.com/blI0oRkfN8
— Dunja Mijatovic (@Dunja_Mijatovic) 11. August 2017
Should the UK/EU/USA ban companies from doing business with Burma’s military? https://t.co/OywYCPZyTz
— Burma Campaign UK (@burmacampaignuk) 17. Juli 2017
Contributing to #GlobalGoals by providing youth with tools to promote respect for the rule of law https://t.co/7WGCdw41yD #Education4Justice pic.twitter.com/GC7nphBs4L
— UN Vienna (@UN_Vienna) 12. August 2017
Smiles on kids‘ faces during visit of Clowns w/o Borders to @MSF center in #MajdalAnjar is contributing to their health & lives@MSF_Lebanon pic.twitter.com/3rHfNaAhe1
— Lotte Leicht (@LotteLeicht1) 12. August 2017
Israeli 19-year-old jailed for refusing military service https://t.co/mgTTbg98U9
— Michael Polak (@MichaelPolakLaw) 11. August 2017
#Syria artist is sending shoes to govt leaders, & the message is heartwarming. #Refugees are not numbers, but people https://t.co/LkXXNz6itx pic.twitter.com/ENIrnXTMFi
— Lotte Leicht (@LotteLeicht1) 12. August 2017
“I’m very frightened by the war but I really want to stay in school”
Braving bombs to stay in school in #Yemen https://t.co/Q8akBkFQvy
— Lotte Leicht (@LotteLeicht1) 12. August 2017
15 simple great ideas for #YouthDay to fight corruption like for example, counting school supplies. More >> https://t.co/7xtu3bk4SS pic.twitter.com/2g56dn1jTn
— Transparency Int’l (@anticorruption) 12. August 2017
Celebrating International #YouthDay today, join us in building a #morejustworld for present and future generations pic.twitter.com/MJdEKoDO0b
— Int’l Criminal Court (@IntlCrimCourt) 12. August 2017
Ein Überblick über die Aktivitäten zum Weltflüchtlingstag in ganz Österreich
Are you joining the @RefugeeFoodFest? It’s now an international event taking place in 13 European cities! https://t.co/Qo7jdSUISy
— UN Refugee Agency (@Refugees) 16. Juni 2017
Bravo to #Switerland’s courts for courageously refusing to transfer #refugee to law-breaking #Hungary! https://t.co/FY76r04iq4
— James Hathaway (@JC_Hathaway) 17. Juni 2017
So. Und bevor ich mich weiter ärgere – #twoff.
— Birgit Schmeitzner (@BSchmeitzner) 16. Juni 2017
#Takk & congratulations #Iceland! Sending best wishes to all Icelanders on the National Day!
— Dalia GrybauskaitÄ� (@Grybauskaite_LT) 17. Juni 2017
Estlands Regierungschef fordert Polen, Ungarn und Tschechien zur Aufnahme von Flüchtlingen auf. https://t.co/n34bvztKtb
— ZEIT ONLINE Politik (@zeitonline_pol) 17. Juni 2017
Pakistan says @CIJ_ICJ has rejected India’s appeal for six months‘ time to file plea https://t.co/fHjtHYlbV4 via @timesofindia
— Opinio Juris (@opiniojuris) 17. Juni 2017
Always stay up to date about our events & don’t miss out! https://t.co/OXphkiBX2l pic.twitter.com/GBXEoOOp3u
— UN Vienna (@UN_Vienna) 16. Juni 2017
Get the latest update on the @UN response to the #Syria Crisis: https://t.co/EIqLb3Tb7z pic.twitter.com/SAfznMuui3
— UN Vienna (@UN_Vienna) 15. Juni 2017
New #IMF #socialprotection policy paper ignores evidence inconsistent with #SDGs https://t.co/6YgHapkOBv
— Bretton Woods Proj. (@brettonwoodspr) 16. Juni 2017
Peter Eigen founder of @anticorruption speaks at the opening of #irresistible17 pic.twitter.com/cILHrvyvmx
— Arzu Geybulla (@arzugeybulla) 16. Juni 2017
Cert petition in ATS case against @KBRNewsroom seeks review of potential circuit split in application of Kiobel test https://t.co/ySBZagYXUD
— Julian Ku 古舉倫 (@julianku) 16. Juni 2017
#Schmutzkübelkampagne„- Ung. Regierung kritisiert dt.Medien wg. Todeslaster-Recherchen https://t.co/tXuUTOMzH2
— Stephan Ozsváth, ARD (@ARDOzsvath) 16. Juni 2017
Panel on gender based violence, the crime against humanity of rape as a tool of war, and the justice system @prev_gen pic.twitter.com/YEmMjWSgqX
— CCIJ | CCJI (@CCIJ_CCJI) 15. Juni 2017
Amanda Ghahremani of CCIJ speaking at the Uncondemned parliamentary screening and panel @prev_gen @amandaghahreman pic.twitter.com/co3xflLgsT
— CCIJ | CCJI (@CCIJ_CCJI) 15. Juni 2017
EU-Kommission: Nordstream 2 trägt nicht zu den Zielen der Energieunion bei https://t.co/rTZX1Il70z Dt-russ. Projekt, nix europ. Interessen
— Birgit Schmeitzner (@BSchmeitzner) 16. Juni 2017
Twitter angemacht, Gabriels Irrlichtern gesehen, Kopf geschüttelt https://t.co/M5vZsxn33E #Gazprom
— Birgit Schmeitzner (@BSchmeitzner) 16. Juni 2017
#Bangladesh PM to visit Swedish PM this week. Criticism from Swedish government after my report on RAB in April https://t.co/pkpxKqLZjy
— BeatriceJanzon (@BeatriceJanzon) 12. Juni 2017
=== English below ===
Together with thousands of people worldwide we want to speak up for a humane asylum policy on the World Refugee Day (20 June). Bring umbrellas as a symbol of protection for refugees!
We meet on Tuesday, 20 June at 17.00 at Platz der Menschenrechte near the Marcus Omofuma memorial (Marcus was murdered by three policemen during a deportation in 1999).
We want to form the slogan “Stop deportations” with letters on umbrellas and demand in particular the stop of deportations to Afghanistan by the Austrian government. (People who want to help preparing these umrellas are welcome to help on site at 16.00.)
We also want to take pictures “My voice against racism/for humanity” and collect them for a photo album.
–
#AlBashir case: #ICC Pre-Trial Chamber II to deliver decision on South Africa’s cooperation on 6 July 2017 https://t.co/pGDXy1OvtT pic.twitter.com/4Qqk7u1KAG
— Int’l Criminal Court (@IntlCrimCourt) 16. Juni 2017
Farce: Turkey breaks #InternationalLaw, sentences U.N. war crimes judge on ‚terrorism‘ charges https://t.co/vkBb4LIaOd #MICT #INjustice
— Mark Kersten (@MarkKersten) 16. Juni 2017
How international law could scupper a Tory deal with the DUP https://t.co/W2TfTBCxW0 via @ConversationUK
— Opinio Juris (@opiniojuris) 16. Juni 2017
Vorarlberg ist wieder einmal Vorreiter. Dort dürfen Asylwerber jetzt wieder auch von Privaten beschäftigt werden: https://t.co/ITcmMESDxR
— Nina Horaczek (@NinaHoraczek) 16. Juni 2017
Over 350,000 South Sudanese #refugees have made the harsh journey to the Gambella Region of Ethiopia. More info: https://t.co/DGhvGcxUa5 pic.twitter.com/KY6NYLPo4N
— IOM (@UNmigration) 16. Juni 2017
A new Facebook video shows Somalis/Ethiopians #migrants & #refugees abused by gangs in Libya. More info here: https://t.co/qeT76JAJYp pic.twitter.com/Hb7fpBbfFA
— IOM (@UNmigration) 14. Juni 2017
Former #UN SG, Kofi Annan & 9 former African presidents warn that the “future of the #DRCongo is in grave danger“ https://t.co/K53enMKMsZ
— Lotte Leicht (@LotteLeicht1) 16. Juni 2017
Neue Nachbarschaftshilfe wird gut angenommen – https://t.co/E8JRhdUkfWhttps://t.co/MqbYyY43cp @CaritasVbg
— cariklaus (@KlausSchwertner) 16. Juni 2017
Orbán Viktor authorities are really good in harassing opposition parties, NGOs and journalists – doing their… https://t.co/hzVG9t0rRA
— AAH (@AAR_Hun) 16. Juni 2017
Nach Todeslaster-Recherchen:Ung.Regierung kritisiert dt. Medien, János Lázár:“Belastet dt.-ung. Beziehungen„https://t.co/XrAcINzOg2
— Stephan Ozsváth, ARD (@ARDOzsvath) 16. Juni 2017
Video „Aggressiv und rücksichtlos: Das brutale Vorgehen der libyschen Küstenwache“ – Monitor https://t.co/Nf3V3I9MAU via @ARDde
— Lotte Leicht (@LotteLeicht1) 16. Juni 2017
‚I Saw My City Die‘
17.5 million people have been displaced in #Yemen, #Syria & #Iraq.
Devastating new @ICRC report: https://t.co/s3ZqLLPWhT pic.twitter.com/NtrBqAfu9y— Lotte Leicht (@LotteLeicht1) 16. Juni 2017
„I’m not a number, I’m a person.“
Watch & learn from the inspiring @NujeenMustafa who fled #Syria in a wheelchair https://t.co/14ZcDTaHUV— Lotte Leicht (@LotteLeicht1) 16. Juni 2017
From Syria to Germany in a wheelchair. Nujeen’s story: https://t.co/UrFUPGJDnM pic.twitter.com/h98icwdxft
— UN Refugee Agency (@Refugees) 16. Juni 2017
Cities have become war’s new front lines: https://t.co/cAq46Kw6Ob pic.twitter.com/xcF0bKzwG3
— ICRC (@ICRC) 16. Juni 2017
It could be you & your family#Syria artist Abdulla Al-Omari gives world leaders a makeover&paints them as #refugees https://t.co/sGFv8aeBw8 pic.twitter.com/m0MTwQLquW
— Lotte Leicht (@LotteLeicht1) 16. Juni 2017
Come on, @IntlCrimCourt, the English version of the #Ntaganda 2nd arrest warrant decision is the French one… @ICC
— Kevin Jon Heller (@kevinjonheller) 16. Juni 2017
#ArchivesGouv
Le 16 juin 1944, Marc Bloch, historien français et héros de la Résistance est exécuté par la Gestapo 👉🏼https://t.co/xIg7brvgAD pic.twitter.com/nqKDPORzLM— Gouvernement (@gouvernementFR) 16. Juni 2017
UN treaty to ban nuclear weapons may be adopted soon https://t.co/oPqQtwW8y3
— Jutta Brunnée (@JuttaBrunnee) 16. Juni 2017
Germany, Austria Charge U.S. Senate’s Russia Sanctions Bill ’s ExtraTerritorial Reach Wd Violate Intl Law https://t.co/CYwIoUnm7B via @WSJ
— Opinio Juris (@opiniojuris) 16. Juni 2017
Breaking: Turkey summons US ambassador after D.C. police issue arrest warrants for 12 members of Erdogan’s security detail.
— Piotr Zalewski (@p_zalewski) 15. Juni 2017
My long explanation @opiniojuris of why the Appeals Chamber’s new war-crimes judgment is wrong. https://t.co/xxsxqlQA43 #ICC #Ntaganda #IHL
— Kevin Jon Heller (@kevinjonheller) 15. Juni 2017
Swiss banks lobby for get-out clause as „end of bank secrecy“ nears https://t.co/I4vw4Ym2r9 Using that old bullshit excuse
— Nicholas Shaxson (@nickshaxson) 16. Juni 2017
#Maldives cableTV provider @Medianetmv fined US$35k for airing „Stealing Paradise“ by @AJEnglish & @willjordan https://t.co/6fF7iqADez 1/2 pic.twitter.com/rZphrLXgi4
— Transparency Int’l (@anticorruption) 16. Juni 2017
New @kevinjonheller Post: @IntlCrimCourt Appeals Chamber Holds That A War Crime Does Not Have to Violate IHL https://t.co/nf9tnHbMOj
— Opinio Juris (@opiniojuris) 15. Juni 2017
Victory for Roma in Macedonia! Government to pay compensation for Roma prison death, amidst spate of similar cases. https://t.co/0QFH5l2sRx pic.twitter.com/FJX2YjXk78
— ERRC (@ERRCtweets) 15. Juni 2017
Is the Commission serious about Roma inclusion in the Western Balkans? Read more in our latest blog https://t.co/1N0IgzVXRR pic.twitter.com/xwKv85Rzl6
— ERRC (@ERRCtweets) 15. Juni 2017
We kept him in a coma–cut off from consular visits and vital medical assistance for a year–on „humanitarian grounds“. pic.twitter.com/gWtoPCqnsJ
— Curtis Melvin 커티스 멜빈 (@CurtisMelvin) 15. Juni 2017
News Lens: International Finance Corporation flashes warning signs for Green Climate Fund https://t.co/dfktnCLOoE
— Bretton Woods Proj. (@brettonwoodspr) 15. Juni 2017
Aufruf: Österreichweite Mahnwachen „Lichter gegen Abschiebungen“
#
.

Get the latest update on the @UN response to the #SyriaCrisis https://t.co/ZOqtBtd8Cq pic.twitter.com/evTLrWkfkX
— UN Vienna (@UN_Vienna) 10. November 2016
Did you know that we also tweet in German, Hungarian, Slovak and Slovene? Follow us @UNO_Wien @ENSZ_Becs @OSN_Vieden @ZN_Dunaj !
— UN Vienna (@UN_Vienna) 8. November 2016

#Vote2016 #ElectionDay pic.twitter.com/OcZMazCbdt
— ACLU National (@ACLU) 8. November 2016
21:44 Die Anruferin hat dem Obdachlosen vermutlich das Leben gerettet. Wir bringen ihn jetzt in ein Notquartier. #kaeltebus #caritas #wien
— cariklaus (@KlausSchwertner) 8. November 2016
20:34 Immer wieder läutet das Kältetelefon. Jetzt hat gerade eine Frau angerufen und uns auf 1 Obdachlosen im 22. Bezirk aufmerksam gemacht.
— cariklaus (@KlausSchwertner) 8. November 2016
g

Proper shelter from the cold needed. No excuse for #EU failure to provide humane reception conditions to #refugees https://t.co/H3IcEnQ1l2
— Lotte Leicht (@LotteLeicht1) 8. November 2016
Today is the anniversary of the #RabaaMassacre
Today is the anniversary of the #RabaaMassacre in which #Egypt junta killed 1000+ protesters in 1 day #RememberRabaa pic.twitter.com/rOLbeSXNXa
— Middle East Monitor (@MiddleEastMnt) 14. August 2016


August 14, 2013 will forever be a dark spot in Egypt’s history. And no, you’ll never be able to justify the massacre of 1000 human beings.
— Dalia Ezzat (@DaliaEzzat_) 14. August 2016
#FreeShawkan in my thoughts today on the 3rd anniversary of day when he should never have been arrested at all! @CiLuna27 @ShawkanZeid
— Kate (@Beerinwitsout) 14. August 2016
It is looking increasingly likely that Brexit will never happen: https://t.co/cyYSOztJxC
— Opinio Juris (@opiniojuris) 14. August 2016
Back to Brist pic.twitter.com/vAu7hGdlUL
— Toby Cadman (@tobycadman) 14. August 2016
Bangladesh: End Illegal Detentions https://t.co/voyUJQ8FNZ
— Toby Cadman (@tobycadman) 14. August 2016
The case for Israel and the legality of the Balfour Declaration https://t.co/C5FDaPDL8m via @fullcomment
— Opinio Juris (@opiniojuris) 14. August 2016
Sorting (secret) fact from (WikiLeaked) fiction about former low-level Gitmo detainees https://t.co/tvIwcCCvjC
— Charlie Savage (@charlie_savage) 13. August 2016
#Egypt should pass transitional justice law and compensate victims of #Rabaa massacre –@HRW https://t.co/7HpchCiOCr
— Mona Eltahawy (@monaeltahawy) 14. August 2016
Majlinda Kelmendi brings home to #Kosovo her golden medal in #Judo from #Rio2016 She received a heroine’s welcome! pic.twitter.com/CxizN4ZRax
— Lirim Greiçevci (@AmbLirim) 14. August 2016

Doctors Without Borders (MSF) said victims of air strike in Yemen were school children aged eight to 15 years https://t.co/g9ozxXNKss
— Al Jazeera News (@AJENews) 14. August 2016
La France en or, grâce à @piconcharline!
Toutes mes félicitations #Rio2016 https://t.co/UtbYnIENWT— Gérard Larcher (@gerard_larcher) 14. August 2016
I follow @ahmedshaheed & @JBI_HumanRights for updates on international human rights law, especially at UN level #ScholarSunday
— Rosa Freedman (@GoonerProf) 14. August 2016
Australia ‚has lost moral compass‘ over immigration detention: New Zealand opposition https://t.co/j4mMgohNpr via @smh
— Sonya Sceats (@SonyaSceats) 14. August 2016
#Goal1: Kick #poverty to the curb! Who needs it anyway? https://t.co/sKSVCoM8R0 #Pandas4GlobalGoals pic.twitter.com/uCwhFAulml
— UN Vienna (@UN_Vienna) 14. August 2016

„Ich würde viel lieber arbeiten, als mit 800 Euro zu Hause zu sitzen“
Ich würde mir wünschen, dass die… https://t.co/BnKHhzzdwR
— cariklaus (@KlausSchwertner) 14. August 2016

3rd #suspension #bridge on the #Bosphorus in #Istanbul will be opened on 26th of August 2016 https://t.co/r6k01sOYbe pic.twitter.com/i6dizqaukT
— Burak Sansal (@allaboutturkey) 14. August 2016
#Ethiopia’s int‘ donors should insist on int’l investigation into govt abuses killing up to 100 unarmed protesters.https://t.co/skG6KTEGOx
— Lotte Leicht (@LotteLeicht1) 14. August 2016
.@MSF received today 21 injured & 10 deaths in Haydan #Saada. All were under 15 years old. #Yemen pic.twitter.com/LVYzsBKVAa
— أطباء بلا حدود-اليمن (@msf_yemen) 13. August 2016
Hear, hear! An excellent suggestion @Charlie_Savage Great to see the years of #Gitmo misinformation being challenged https://t.co/EH8iBAADOL
— Laura Pitter (@Laurapitter) 13. August 2016
#UN @Refugees agency seriously concerned about reported sexual assaults on children at Greek refugee camps#Refugees https://t.co/VW3ABbFJBb
— Lotte Leicht (@LotteLeicht1) 14. August 2016
Follow due process. Investigation of #ThailandAttacks is not an excuse for arbitrary arrest, secret detention & other abuses by authorities.
— Sunai (@sunaibkk) 14. August 2016
U.N. rights boss decries purge in Turkey, voices concerns on China ………Zeid, turning to repeat presidential elections in Austria set for October, added: „If the head of the Freedom Party should win, Norbert Hofer, I think it’s a real turning point on the European stage and could have consequences well beyond Austria.“https://t.co/1HzIhRRkI4 via @Reuters
— Benedict Rogers (@benedictrogers) 13. August 2016
Air strike on school in Yemen leaves at least 10 children dead https://t.co/FVg0H4w46K pic.twitter.com/MpL4xRBG0J
— SBS News (@SBSNews) 13. August 2016

#UPDATE THE CONCERN IS RISING UP REGARDING @MaythamAlsalman#Bahrain #BRN #Manama pic.twitter.com/pFjntcmUQZ
— LuaLuaTV (@LuaLuaEnglish) 14. August 2016
Swiss party submits petition for referendum on domestic courts‘ sovereignty over intl law. https://t.co/qXoVXOeaW3
— Opinio Juris (@opiniojuris) 13. August 2016
Bezahlt? Bonze.
Unbezahlt? Glaub ich nicht.
Privatwirtschaft? Korrupt.
Öffentlich? Versorgungsposten.
In Österreich? Freunderlwirtschaft.
International? Davongelaufen.
Reich? Hat sicher was gestohlen.
Arm? Unfähig.
Es gibt Menschen, die gäbe es am besten nicht.
Und selbst dann wäre es verdächtig.
https://www.un.org/press/en/2016/sga1675.doc.htm ….
— Matthias Euler-Rolle (@eulerrolle) 13. August 2016
I remember when ppl argued in Jan 2012 that military action against Assad would make things worse. 5000 had been killed. Now it’s 470,000.
— Shadi Hamid (@shadihamid) 13. August 2016
News Lens: Lauding India, IMF calls for budgeting to bridge gender gap
Heading to Geneva for meetings at the UN
— Toby Cadman (@tobycadman) 11. August 2016
.@opiniojuris Good news for UK human rights architecture + #GoodFridayAgreement – but attacks on #Strasbourg Court are likely to continue
— Tom Gerald Daly (@DemocracyTalk) 11. August 2016
Somali pirates get five years in jail https://t.co/Asu8D1NazM h/t @mary_harper
— OCEANUSLive.org (@OCEANUSLive) 11. August 2016
New Emerging Voice Post: A Case of Firsts for the ICC, Destruction of Cultural Heritage as a War Crime https://t.co/Cf0rvZQ6Ud
— Opinio Juris (@opiniojuris) 11. August 2016
#Goal5: Women & girls have something to say! Stop, listen &
celebrate https://t.co/0FNnZ20NqZ #Pandas4GlobalGoals pic.twitter.com/LPik7U8jLu— UN Vienna (@UN_Vienna) 11. August 2016
1 Ereignis – 2 Medien – 2 Artikel https://t.co/eGYBFNCah1 https://t.co/HLpONErkWP
— cariklaus (@KlausSchwertner) 11. August 2016
@FreeEgyptPress @ShawkanZeid @AlsisiOfficial #FreeShawkan Mr President urge you 2 order this man’s release. You can give him his life back!
— Kate (@Beerinwitsout) 11. August 2016
Chlorine gas from a barrel bomb attack against the City of Aleppo leaves at least three dead and dozens critical. pic.twitter.com/vFcrw2JtcQ
— SBMS (@SyrBritMedSoc) 11. August 2016
Chlorine attack Aleppo @UOSSM report 3 dead inc woman & son many treated at area hospitals At least 10 victims under 10 &
25 under 5 yrs old— Hamish DBG (@HamishDBG) 11. August 2016
UK PM Theresa May is ’set to shelve‘ David Cameron’s flagship plan for British Bill of Rights https://t.co/E0CG3m6bFU
— Opinio Juris (@opiniojuris) 11. August 2016
#شاهد:
(فيديو) العودة يحذر مجاهدي سوريا: إياكم والتنازع https://t.co/GuzYsbd38n@salman_alodah pic.twitter.com/NEHHhRilHR— منتدى العلماء (@MuntadaAlulama) 3. August 2016

News Lens: Lauding India, IMF calls for budgeting to bridge gender gap https://t.co/wuHGKgcT56
— Bretton Woods Proj. (@brettonwoodspr) 11. August 2016

News Lens: Greek Crisis, the book. Or actually several of them. https://t.co/f8X00uIK47
— Bretton Woods Proj. (@brettonwoodspr) 11. August 2016
Get the latest update on the @UN response to the #Syria Crisis https://t.co/ZOqtBtd8Cq
— UN Vienna (@UN_Vienna) 11. August 2016
#Oman detains journalists covering #corruption + shuts down media outlet, via @AmnestyOnline https://t.co/qinloTwvLf #pressfreedom
— Transparency Int’l (@anticorruption) 11. August 2016
2MRW, 14.30 (CEST): @UNYouthEnvoy hosts FB chat on role of youth in promoting peace & sec. https://t.co/K19cn1uhOv pic.twitter.com/w1R7pW9tYC
— UN Vienna (@UN_Vienna) 11. August 2016

Make sure to dispose of your rubbish properly at #Rio2016: https://t.co/OFPD4f3wQC#GreenPassport pic.twitter.com/IecHJ5y3VW
— UN Vienna (@UN_Vienna) 11. August 2016
Syrien-Krieg: Ärzte melden Gasangriff auf Aleppo … https://t.co/FdK6m0YKox
— SPIEGEL Politik (@SPIEGEL_Politik) 11. August 2016
#ZambiaDecides today as citizens head to vote for new leader! Top concern: “runaway #corruption” hurting economy. https://t.co/1ryQc4MC7X
— Transparency Int’l (@anticorruption) 11. August 2016

ERRC uncovers grim reality of access to water for Roma in Ukraine https://t.co/huRuAFDyQ1 pic.twitter.com/AphZ09FnGK
— ERRC (@ERRCtweets) 11. August 2016

Muslims attend Catholic mass in Prague, condemn IS. Church full, hate-monger protest outside https://t.co/t3K82exk5a pic.twitter.com/XCwegQB86W
— Andrew Stroehlein (@astroehlein) 11. August 2016

Europe’s largest travel agent TUI hit by rising terrorism fears among holidaymakers https://t.co/Lm2gRyTCWF
— The Independent (@Independent) 11. August 2016

An ex-EU top-dog turned corporate fat cat? Call him out & block the #revolvingdoors https://t.co/W3XNNWLkse #Barroso pic.twitter.com/Vzw7PY8ZQ4
— CEO (@corporateeurope) 11. August 2016
#Ukraine Pres confirms he WILL launch anti-corruption tool on 15 August! All eyes watching! https://t.co/YwFVw9g0F5 pic.twitter.com/3dWOsUBBRf
— Transparency Int’l (@anticorruption) 11. August 2016
Nearly 6,000 “ghost workers” removed from #Uganda government payroll. Time to fight endemic #corruption! https://t.co/7dxEVWkWek
— Transparency Int’l (@anticorruption) 11. August 2016

Leaked #NauruFiles show horrors of shameful #Australia #refugee detention system. Close it! https://t.co/MJwBnRe6Xk pic.twitter.com/mU7nUv7qHk
— Lotte Leicht (@LotteLeicht1) 11. August 2016

Our petition to block the EU #revolvingdoor & stop #Barroso is sky-rocketing. Ready to push? https://t.co/W3XNNWLkse pic.twitter.com/roRNgZ64KJ
— CEO (@corporateeurope) 11. August 2016
BBC News – Councillor in Aleppo: ‚We can hear the war all around‘ https://t.co/gACyg0JXXB We are completely starved
— Hamish DBG (@HamishDBG) 10. August 2016
What’s a Blue Community? Join @cupenat @EauSecours @CouncilofCDNs @fsm2016wsf tomorrow to find out! https://t.co/2fBu59QQm6 Protect #water!
— Emma Lui (@EmmLui) 11. August 2016
Falcon Private Bank touchée par le scandale financier 1MDB – Le Temps https://t.co/AWq54282AY
— Hans-Rudolf Scheller (@schellerfamily1) 11. August 2016
Des drones traquent les fraudeurs fiscaux – Le Temps https://t.co/Ke24hmIJDy
— Hans-Rudolf Scheller (@schellerfamily1) 11. August 2016
#FACT 1.8 billion people live below a moderate #poverty threshold of US$2.50/day #DGFF2016 https://t.co/mfKyWtJAel … pic.twitter.com/txseknYVAT
— UNCTAD (@UNCTAD) 11. August 2016
#Aleppo – UNO: Drei Stunden Feuerpause reichen nicht https://t.co/yKbQgQgmv8
— cariklaus (@KlausSchwertner) 11. August 2016

Joint force: With hundreds of NGOs frm @ALTEREU, citizens & @wemoveEU against #EU #revolvingdoors and #Barroso. https://t.co/bcI4TKb0Qv
— CEO (@corporateeurope) 10. August 2016
Mad about #Barroso&Co moving from @EU_Commission into corp. jobs to cash in their influence? https://t.co/W3XNNWLkse pic.twitter.com/YYe3RrguWd
— CEO (@corporateeurope) 11. August 2016
Back transparent,fully independent decisions on #revolvingdoors &sanctions for rule breakers https://t.co/W3XNNWLkse pic.twitter.com/fohqFtOupx
— CEO (@corporateeurope) 11. August 2016
World Bank and IMF: Where do they stand on progressive and responsible taxation?
@HamishDBG sadly and tragically Hamish they aren’t listening. Or if they are they have yet to act. And they may not. #medicsunderfire
— Saleyha Ahsan (@SaleyhaAhsan) 5. August 2016
#Egypt The case of young journalist @FreeFakharany, 3 years in prison, his life stolen: https://t.co/qZlrIOPwi4 pic.twitter.com/7z8sv6AAs0
— Pressbehindbars (@FreeEgyptPress) 5. August 2016
Yusra swam to reach safety after fleeing Syria. Now she’s going to swim at the #Rio2016 @Olympics. #TeamRefugees pic.twitter.com/6jj76O3mB2
— UN GA President (@UN_PGA) 5. August 2016
Important piece:Teen Executed for Gay Sex in Iran Is Latest in Long Trend. With video of @ahmedshaheed cc: @matbreen https://t.co/aIiy2POUxz
— Benjamin Weinthal (@BenWeinthal) 5. August 2016
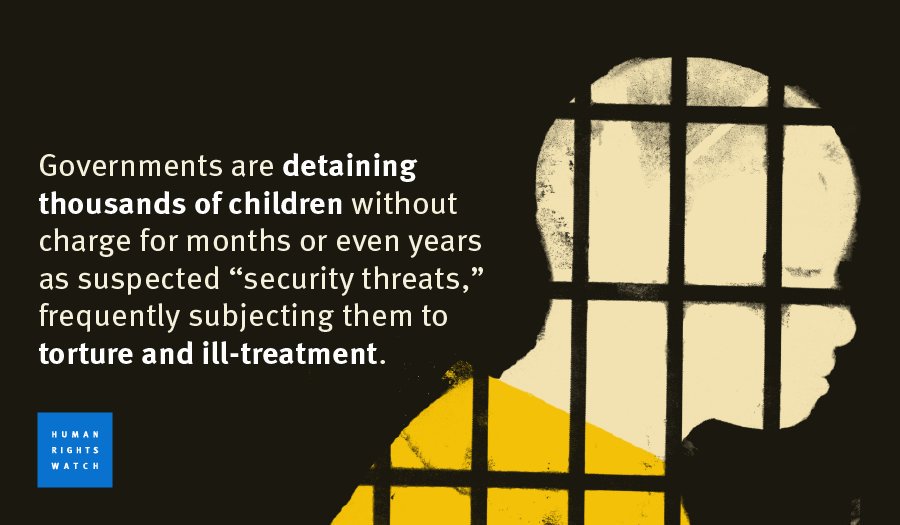
Heart-wrenching video about 14-year-old Ahmad, detained in #Syria.@ajplus @HRWhttps://t.co/iN9lqM4UcR … pic.twitter.com/plf2wFVmYY
— Lotte Leicht (@LotteLeicht1) 5. August 2016
Stand w/ @hrw @amnesty @pressfreedom @PENamerican against #TurkeyPurge of scholars, media https://t.co/mkDnl1XJfl pic.twitter.com/iVWH5XrKfH
— PENamerican (@PENamerican) 5. August 2016
U.S. Not Persuaded to Extradite Imam Over Turkey Coup https://t.co/bfKIlYSvkC
— Opinio Juris (@opiniojuris) 5. August 2016
New Guest Post: The International Criminal Court at 14 https://t.co/KIJOQpGjnB By fmr @ukintllaw counsel @shehzad55 — Opinio Juris (@opiniojuris) 4. August 2016
Ayatollah Khamenei Addresses Tehran Prison Mess Hall During Annual Press Correspondents’ Dinner https://t.co/uLrfnJz2Ni — The Onion (@TheOnion) 5. August 2016
Provincial government confirms another pipeline spill in Saskatchewan. Details here: https://t.co/dJhSl1H6Jr @CBCAlerts @CBCSask
— Devin Heroux (@Devin_Heroux) 5. August 2016
„Es geschehen Kriegsverbrechen, die einem den Atem rauben.“ #Aleppo #syrien https://t.co/qGSHPU01Dw @WienerZeitung @petraramsauer
— cariklaus (@KlausSchwertner) 5. August 2016
EU’s reaction to recent execution of 20 Sunnis by #Iran https://t.co/tZHdvhSGZV — Golnaz Esfandiari (@GEsfandiari) 5. August 2016
Process on enacting #Maldives Defamation Bill:- 1-Govt draft bill 2-Get opinion of #Figh #Academy 3-Take vote at #Majlis floor. — Hassan Latheef (@HassanLatheef) 5. August 2016
U.N. rights boss says executions in Iran were ‚grave injustice‘ https://t.co/Ll87F16VyK via @Reuters
— Golnaz Esfandiari (@GEsfandiari) 5. August 2016
Bernard Rorke looks at Hungarian role in #romagenocide, anniversary of #neonazi murders and #holocaustdenial https://t.co/arazyXHOh7
— ERRC (@ERRCtweets) 5. August 2016
And if members of a government try to control Islam, then what use is a Fiqh Academy? Separation good for both. https://t.co/qBBNJdnvZw — CIRF (@IslamAndRF) 5. August 2016
The press freedom crackdown after the #TurkeyCoupAttempt continues. Stay up to date with our Crackdown Chronicle:https://t.co/NFIvQ9K5vC — CPJ (@pressfreedom) 5. August 2016
Joseph Stiglitz resigns from Panama Papers committee over ‘censorship’ https://t.co/UXIFzD1PeN
— The Globe and Mail (@globeandmail) 5. August 2016
„Proposed law on contempt of court threatens press freedom in Singapore“ https://t.co/Z4z1ShYy7f
— Progressive Lawyer (@ProgLawyer) 5. August 2016
“Fear still rules in #Gambia.” Daughter of politician who died in police custody @newsweek https://t.co/Bjtcm81cR1 pic.twitter.com/PmAvsFlzf4 — Lotte Leicht (@LotteLeicht1) 5. August 2016
Nobel economist Stiglitz resigns from Panama transparency commission https://t.co/f1JcE0i1r9 via @ReutersIndia — Hans-Rudolf Scheller (@schellerfamily1) 5. August 2016
#Armenia police response to peaceful protests has been excessive & cruel. #EU shld insist on fair trials & releases https://t.co/2zvrGRSYp4
— Lotte Leicht (@LotteLeicht1) 5. August 2016
Final preparations – Yiech starts in 800m-running for the first-ever „Refugee Olympic Team“. #docuimage @RNDnewsroom pic.twitter.com/UJW3nc3MxM
— Isa Lange (@stadtmaulwurf) 5. August 2016
Panama Papers – Panama Papers: Expertenausschuss ist gescheitert – Süddeutsche.de https://t.co/GW3SDZM5He #PanamaPapers — Panama Papers (@panamaspapers) 5. August 2016
Latin American tax clampdown latest threat to Swiss bank accounts https://t.co/cbgPFLHLFm via @Reuters — Tax Justice Network (@TaxJusticeNet) 5. August 2016
This lack of transparency in #UNSC straw polls is undignified for @UN & #UNSGcandidates Stmt https://t.co/fPN0ZuKXeT pic.twitter.com/rKM1YSSx9S
— UN GA President (@UN_PGA) 5. August 2016
„Cruel in the extreme“: #Australia accused of ignoring appalling abuse of #refugees. @washingtonpost on AI/@HRW rpt https://t.co/Ajsafh3e4v
— Lotte Leicht (@LotteLeicht1) 5. August 2016
„I thought I will die soon.“ This doctor survived the U.S. Air Force bombing of an @MSF hospital: https://t.co/sLp2ACZxUJ — AJ+ (@ajplus) 4. August 2016
„Fluchtkorridore aus #Aleppo sind eine Finte – sie führen in die Hände des Assad-Regimes“, berichtet die Aktivistin @HaymaAlyousfi — Ö1 Journale (@oe1journale) 4. August 2016
Traveling to #Rio016? Fewer stops mean lower emissions. https://t.co/OFPD4f3wQC#GreenPassport pic.twitter.com/Fextf0kxgT
— UN Vienna (@UN_Vienna) 5. August 2016


Thanks to all #VIMUN participants standing up for the #GlobalGoals @UN_Vienna https://t.co/cz8KVDpZra @GlobalGoalsUN pic.twitter.com/8IQRqCJJSS
— UN Vienna (@UN_Vienna) 5. August 2016
The World Bank’s failed accountability experiment: Why the Inspection Panel’s ‘Pilot’ should dead end https://t.co/9jahSbynnU — Bretton Woods Proj. (@brettonwoodspr) 5. August 2016
World Bank and IMF: Where do they stand on progressive and responsible taxation? https://t.co/QPBh9e90iB — Bretton Woods Proj. (@brettonwoodspr) 5. August 2016

Meet the 10 members of #TeamRefugees who will compete at #Rio2016 under the @Olympics flag https://t.co/favCcRlLBU pic.twitter.com/yDqOQpoK8Q — UN Vienna (@UN_Vienna) 5. August 2016
J’ai écris à @manuelvalls pour lui demander d’associer le parlement aux réflexions sur la place de l’Islam en France https://t.co/1pu1rurqb8 — Gérard Larcher (@gerard_larcher) 5. August 2016
#Goal10: Equal incomes for all! Religion, gender, etc. shouldn’t matter https://t.co/1XRepjWjT5 #Pandas4GlobalGoals pic.twitter.com/z8qkPqIMY3 — UN Vienna (@UN_Vienna) 5. August 2016
Ban Ki-moon receives Olympic torch from IOC President Thomas Bach. #Rio2016 pic.twitter.com/X7fnW1yE18 — UN Spokesperson (@UN_Spokesperson) 5. August 2016

Coming up today: second round of #UNSC straw polls on #UNSGcandidates. pic.twitter.com/slkZ7FjTOL — UN GA President (@UN_PGA) 5. August 2016

What to think when #Russia walks into the #Olympics stadium? @panfilova’s answer: https://t.co/no1ni4zkJ4 #Rio2016 pic.twitter.com/SJVTR31RAd — Transparency Int’l (@anticorruption) 5. August 2016
Deutschland erleichtert Flüchtlingen den Zugang zum Arbeitsmarkt: https://t.co/CJmtk9awTU — derStandard.at (@derStandardat) 5. August 2016
#Argentina needs leadership in the fight against corruption, @JoseUgazSM said to @mauriciomacri pic.twitter.com/RzSyDNzEkT — Transparency Int’l (@anticorruption) 5. August 2016
Steueramnestiegesetze: Schweizer Banken droht weiterer Milliarden schwerer Aderlass https://t.co/rikaRcx55T — WirtschaftsBlatt (@wiblatt) 5. August 2016
Cappadocia in 1962 https://t.co/0kq7MMd3eN — Burak Sansal (@allaboutturkey) 5. August 2016

Istanbul, Turkey. Hi-res here: https://t.co/sLGHatGQbP pic.twitter.com/nMFcsdQbIq — Jeff Williams (@Astro_Jeff) 3. August 2016
@UNHumanRights To kick off 2016, #SaudiArabia executed 47 people including #SheikhNimr. #Iran is making sure there’s competition — Nicolas Agostini (@Nico_Agostini) 5. August 2016
U.N. rights boss says executions in Iran were ‚grave injustice‘ https://t.co/hucx4rzQhs via @Reuters — Death Penalty Info (@InfoPenalty) 5. August 2016
BBC News – Iran’s Rouhani shelves civil service exam over female discrimination https://t.co/BwMDhZDSaq — Ahmed Shaheed (@ahmedshaheed) 5. August 2016
#Iranian Political Prisoners in a letter to #UN officials & Int community: Do something to stop executions in #Iran. @ahmedshaheed @amnesty — United for Iran (@united4iran) 5. August 2016
‚Dead souls in living bodies‘: Australia accused of abusing refugees @CNNI https://t.co/WL37WP1rwX — Ahmed Shaheed (@ahmedshaheed) 5. August 2016

Scenes of medieval horror as #Philippines ‚war on drugs‘ worsens jail miseries, by @condeHRW https://t.co/q90qlIezsg pic.twitter.com/DdT8w88DF3 — EmmaDaly (@EmmaDaly) 3. August 2016

The Plaza @UN_Vienna this morning. Visit us and see for yourself #UNToursVienna https://t.co/2QGRugl0N5 pic.twitter.com/rvmhpVj15x — UN Vienna (@UN_Vienna) 5. August 2016
Report of UN SR on Freedom of Expression on his visit2 #Maldives in 2009. Guard against enemies of #opensociety.https://t.co/Z1u5uGvKZf — Ahmed Shaheed (@ahmedshaheed) 5. August 2016
Appalled by the continuing high rate of executions in the Islamic Republic of Iran! pic.twitter.com/sjyYrbXZAt — Ahmed Shaheed (@ahmedshaheed) 5. August 2016
Outrageous! Iran executes gay teenager for crime he allegedly committed as a juvenile https://t.co/vz8L5SlQ40
— Ahmed Shaheed (@ahmedshaheed) 5. August 2016
Results of our work in Iraq unveiled: Bringing IS slavers to justice https://t.co/ZAGsybalkl
— Nerma Jelacic (@NermaJelacic) 3. August 2016
Schweizer Banken droht weiteres Ungemach https://t.co/FftrYx4loJ pic.twitter.com/bebFenwxGL — Hans-Rudolf Scheller (@schellerfamily1) 5. August 2016
#Rio2016 about to start! Our take on corruption in #Brazil & #Olympics and how to stop it: https://t.co/OreiU0kpkx pic.twitter.com/OHG4bGYYSy — Transparency Int’l (@anticorruption) 5. August 2016
For the first time in our history, American families have more student debt than credit card debt. That is an extraordinary reality.
— Bernie Sanders (@BernieSanders) 4. August 2016
Tous derrière la #FranceOlympique et notre porte drapeau @teddyriner En route pour les médailles
— Gérard Larcher (@gerard_larcher) 5. August 2016
Some of the unaccompanied minors crossing the #Med in boats like this have been just 8 years old pic.twitter.com/vqsSdBPcIQ — MSF Sea (@MSF_Sea) 5. August 2016
President Obama writes essay on feminism and calls on men to fight sexism https://t.co/R6Ekz5Md0b pic.twitter.com/rtUcZtyd5L — The New York Times (@nytimes) 4. August 2016
Medienbericht: Zahl der Asylbewerber aus der #Türkei steigt https://t.co/zixjSEJnBO via @SPIEGELONLINE
— Lotte Leicht (@LotteLeicht1) 5. August 2016
#SouthSudan fighting resulted in widespread sexual violence, incl rape by soldiers&men in plain clothes,#UN HR Chief https://t.co/k6hB4cC0vg
— Lotte Leicht (@LotteLeicht1) 5. August 2016
#Turkey: Thousands of academics fired. Dozens of journalists arrested. End #TurkeyPurge https://t.co/v8D63Qj9W0 … pic.twitter.com/tjrlD5PaBT
— Lotte Leicht (@LotteLeicht1) 5. August 2016
Wir sind heute fast ausgebucht!!! Wer trotzdem vorbeikommen will, heute Abend ist wieder ab 21 Uhr Sommerkino bei… https://t.co/zyGVIaBcKR
— cariklaus (@KlausSchwertner) 5. August 2016
Is Australia ignoring abuses against asylum seekers? https://t.co/HYQRpZleE3
— AJ+ (@ajplus) 4. August 2016
Join @PENamerican, @Amnesty & @HRW, and demand #Turkey ends its attacks on free expression https://t.co/we0VQ0D9cq pic.twitter.com/I1zVRxfYD0
— Lotte Leicht (@LotteLeicht1) 5. August 2016
#Saudi women can climb the highest peaks;High time Govt drops all ridiculous sports barriers https://t.co/cxdQ3zhrbf pic.twitter.com/VQwMxVDcLx
— Lotte Leicht (@LotteLeicht1) 5. August 2016
Atomic Bomb Awareness Day commemoration now @UN_Vienna – @UN_Disarmament @DNPEduPartner pic.twitter.com/DiATHYrqmi
— UN Vienna (@UN_Vienna) 5. August 2016
Say never again to Hiroshima and Nagasaki: 12th Genbaku No Hi atomic bombing awareness day @UN_Vienna #Disarmament pic.twitter.com/mOnyF6wC4w
— DNP Education (@DNPEduPartner) 5. August 2016
Compensation deal agreed for Roma victims of holocaust https://t.co/seaFkXU086
— DeinAyurvedaNet2 (@Net2Ayurveda) 5. August 2016
#Onthisday 80 years ago, Jesse Owens won gold in long jump at Berlin 1936 #Athletics https://t.co/JGX0C7DjHT
— Olympics (@Olympics) 4. August 2016
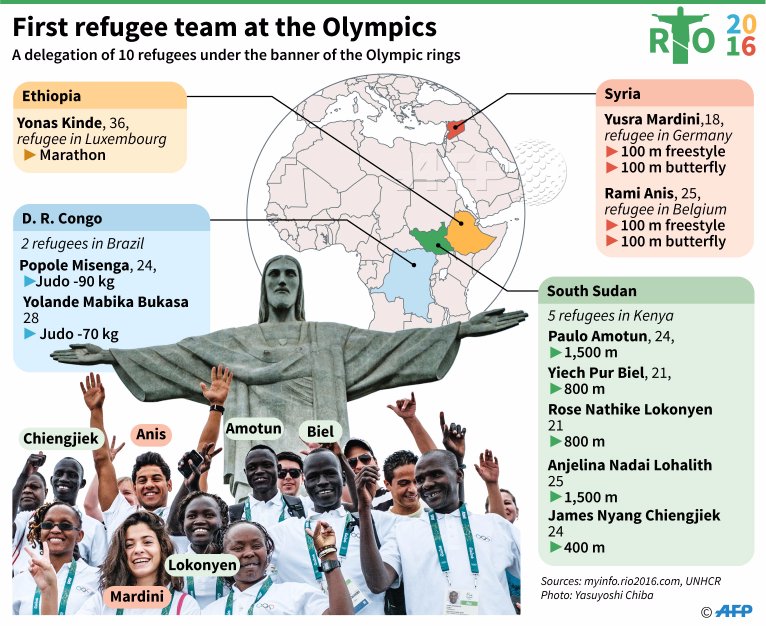
„This is not just a struggle for sport, it’s a struggle for life“ Yolande Mabika #TeamRefugees at #Rio2016
Via @AFP pic.twitter.com/7sHywbHdSd— Lotte Leicht (@LotteLeicht1) 5. August 2016
Bravery across borders. Support #TeamRefugees and stand #WithRefugees everywhere https://t.co/Xp8V4hhB0ehttps://t.co/UjD3OnnYh5
— TeamRefugees (@TeamRefugees) 5. August 2016
Iran execution of a child offender is barbaric and against International law https://t.co/PvUFcVtQ32
— Bianca Jagger (@BiancaJagger) 5. August 2016
Another indictment of #Europe’s cynical policies of walls, rather than solidarity & humanity.#Refugees #Migrants https://t.co/ZD6ihoid74
— Lotte Leicht (@LotteLeicht1) 5. August 2016
Share this video & tell the world that civilians, hospitals, schools, patients, medical staff are #NotATarget.https://t.co/4wVYjZA9Yq
— MSF Canada (@MSF_canada) 4. August 2016
President of @ERRCtweets ÐorÄ�e JovanoviÄ� shares family experience of holocaust on #romagenocide Remembrance Day https://t.co/FRBTuVhKid
— ERRC (@ERRCtweets) 5. August 2016

“Dear refugee sisters & brothers, you are the world’s team. We stand with you.” — Malala’s message to #TeamRefugees pic.twitter.com/schExtBdNt
— Malala Fund (@MalalaFund) 5. August 2016
Today’s Zaman chief editor posts „probably last message“ from her office after police raid
Hear hear https://t.co/xA3PSFmnM7
— Lotte Leicht (@LotteLeicht1) 5. März 2016
Retweeted David Schneider (@davidschneider):
Coquelin! #THFCvAFC #NorthLondonDerby pic.twitter.com/RTPPBLkizm https://t.co/XNjsgqCFiF
— Toby Cadman (@tobycadman) 5. März 2016
A partial & imperfect truce is now in its 2nd week. It’s far less than #Syria needs, far more than it has seen in years. #syriaceasefire
— lyse doucet (@bbclysedoucet) 5. März 2016
Goodnight from #Idomeni where over 12,000 people will spend another cold night including thousands of children pic.twitter.com/XcTKfvHjUa
— MSF Sea (@MSF_Sea) 5. März 2016
„Collective failure to implement measures agreed by #EU led to escalated crisis“ @Refugees https://t.co/1YaftGCFxw pic.twitter.com/2Yva3X1djv
— Lotte Leicht (@LotteLeicht1) 5. März 2016
The #TPP is not a sacred text, need to look at the bugs, says former Foreign Trade director in Globe and Mail https://t.co/jTRU7CF0Og
— Council of Canadians (@CouncilofCDNs) 5. März 2016
Five movies to look out for at the Human Rights Watch film festival https://t.co/G3E3dltUVZ @hrwfilmfestival @HRW pic.twitter.com/sDRgGeZTcR
— Lotte Leicht (@LotteLeicht1) 5. März 2016
#Greece: situation is quickly deteriorating with 30k+ people at border https://t.co/jYTHWESjAA pic.twitter.com/EPrpDDZDK5
— UN Refugee Agency (@Refugees) 5. März 2016
Pebbles arranged by this Syrian sculptor tell moving tales https://t.co/mSCpf3vInQ via @LotteLeicht1 pic.twitter.com/a8KG5bEPp7
— Alex Court (@CourtA) 5. März 2016
Deeply worried over news from Istanbul re court decision & police raid against Zaman newspaper. Another setback for press freedom in Turkey.
— Margot Wallström (@margotwallstrom) 5. März 2016
The #EU continues to call for the immediate release of Nadia Savchenko #freeSavchenko pic.twitter.com/ZD6JQooFrH
— EU Delegation UA (@EUDelegationUA) 4. März 2016
For the first time in years, hundreds used #Syria ceasefire to resume anti-govt protests. https://t.co/Or9mhYtto4 pic.twitter.com/mvgcoMKlbu
— Lotte Leicht (@LotteLeicht1) 5. März 2016
Luftaufnahmen von der Ausnahmesituation in Idomeni. Posted by Stephan Ozsváth on Saturday, March 5, 2016
A team of refugee athletes will be competing at the Summer Olympics in Rio https://t.co/TcMaug9Yk4
— NowThis (@nowthisnews) 5. März 2016
Is Singapore the Next Switzerland for U.S. Tax Crackdown? https://t.co/DusyRVdfix via @business
— Hans-Rudolf Scheller (@schellerfamily1) 5. März 2016
If one disagrees about claims or reports of a newspaper, he should counter them with facts, not by gagging journalism #Zaman
— Martin Schulz (@MartinSchulz) 5. März 2016
Photographer @DanielBiskup’s #Idomeni images show humanity of volunteers, despair of #refugees & #EU govts‘ failure pic.twitter.com/HjFWgqPQJC
— Lotte Leicht (@LotteLeicht1) 5. März 2016
Why so many in #Canada are privately sponsoring #Syria #refugees https://t.co/95EPRGfauC pic.twitter.com/W6KXUBZrYq
— Lotte Leicht (@LotteLeicht1) 5. März 2016
Our logisticians are working hard to put up two more massive tents at #Idomeni. The crowd continues to grow. pic.twitter.com/kMXb9wazvn
— MSF Sea (@MSF_Sea) 5. März 2016
Riot police tear gas supporters of opposition Turkish newspaper #Zaman in #Turkey photo @ozannkosee @AFPphoto pic.twitter.com/YnIsyZexXU
— SundayTimesPictures (@STPictures) 5. März 2016
#EU’s response to #Turkey govt #Zaman takeover. Principled condemnation looks different... https://t.co/Pzt2sxO2il pic.twitter.com/7MDCrgEFW6
— Lotte Leicht (@LotteLeicht1) 5. März 2016
Witness War Is To ‚Experience The Worst In People But To Remember The Beauty‘@lynseyaddario https://t.co/Pu9hzydmd7? pic.twitter.com/J5GVub844l
— Lotte Leicht (@LotteLeicht1) 5. März 2016
If they wanted so much privacy, they shud not have sought elected public office! @IPUparliament @anticorruption https://t.co/4RjlxGHU5M
— ahmed shaheed (@ahmedshaheed) 5. März 2016
„We can’t ignore #immigration when talking about #trafficking. It’s an enormous disincentive for #victims to come forward“ #DoughtyStWomen
— Harriet Johnson (@HarrietEJohnson) 5. März 2016
Refugee boys required surgery after being raped in the Calais Jungle, claim campaigners https://t.co/SWSwBqDpXc
— Daily Mail Online (@MailOnline) 5. März 2016
Supreme Court blocks law limiting abortion access in Louisiana https://t.co/puPOZ0oJxM
— The New York Times (@nytimes) 5. März 2016
In 2016, most UN peacekeepers are from Africa & Asia. In 1995, they were mostly from Europe https://t.co/ycWeeOFpMH pic.twitter.com/xe6Eizior8
— PewResearch Global (@pewglobal) 5. März 2016
„Identifying victims of #trafficking has 2 purposes: protecting victims‘ #humanrights, & enabling prosecution“ Ali Pickup #DoughtyStWomen
— Harriet Johnson (@HarrietEJohnson) 5. März 2016
#Flüchtlinge #Refugees #Turkey
Schüsse bei illegaler Einreise: Türkische Grenzer erschießen offenbar Syrer https://t.co/TANhG5Kx1a #Syria— Muschelschloss ☕ ️ (@Muschelschloss) 5. März 2016
A young girl plays the #violin in #Idomeni today, where 11000 people are stranded according to MSF. #refugeesGr pic.twitter.com/GJ3bh469uZ
— julia druelle (@juliadruelle) 2. März 2016
Schreiben Sie ruhig weiterhin… was und wie wir es wollen #Erdogan https://t.co/j9xU5LEJJr
— cariklaus (@KlausSchwertner) 5. März 2016
The „Barber of #Aleppo“ is bringing dignity back to men trapped in the chaos/mess of #Idomeni with a quality shave. pic.twitter.com/Yj4FEwbomG
— MSF Sea (@MSF_Sea) 3. März 2016
Bürgerkrieg in Syrien: 135 Menschen trotz Waffenruhe getötet ... https://t.co/GUiI3k8Gqa
— SPIEGEL Politik (@SPIEGEL_Politik) 5. März 2016
US @StateDept about #Zaman in #Turkey: „Critical opinions should be encouraged, not silenced“.
What do you think @FedericaMog?— Ricardo Gutiérrez (@Molenews1) 5. März 2016
Meet the widows of #Maidiguri: https://t.co/dBNzOlLLb8 #Nigeria #IWD2016 pic.twitter.com/mmbQsLneo3
— ICRC (@ICRC) 5. März 2016
Le quotidien turc Zaman mis sous tutelle par Erdogan … @SoMabrouk @Perrine_tarneau @Ripamontialbert @publicsenat pic.twitter.com/07bG0ph7XX
— Baudry (@hervebaudry) 5. März 2016
Appalling message by #Germany’s Int Minister in response to #Turkey govt crackdown on rights https://t.co/VDtgBEqbZc pic.twitter.com/K761mQ8zzJ
— Lotte Leicht (@LotteLeicht1) 5. März 2016
State takeover of Turkey’s largest selling newspaper a very ominous step. EU must react strongly. https://t.co/ShLF1kIEZC
— Carl Bildt (@carlbildt) 5. März 2016
The seizure of #Zaman is yet another blow to #pressfreedom in #Turkey. I intend to raise this issue on Monday @Ahmet_Davutoglu
— Martin Schulz (@MartinSchulz) 5. März 2016
Press crackdown could sour #EU–#Turkey summit. EU leaders must respond to seizure of #Zaman https://t.co/fuGGcGRkZD pic.twitter.com/jLIJ53nTn8
— Lotte Leicht (@LotteLeicht1) 5. März 2016
When #EU leaders meet w #Turkey Mon they have to speak out against #Ankara’s press crackdown https://t.co/Sb91l4DgfH pic.twitter.com/gB0NVrl4Jx
— Lotte Leicht (@LotteLeicht1) 5. März 2016
Impartial investigation needed to ensure justice for the killing of activist #BertaCaceres https://t.co/9M7LhIYXGv pic.twitter.com/NBlpENp26X
— Lotte Leicht (@LotteLeicht1) 5. März 2016
HRW says Zaman takeover aims to eradicate opposition, calls on Turkish gov’t to reverse it https://t.co/5Kb8kIjzyu pic.twitter.com/OYZ2OBrQif
— Today’s Zaman (@todayszamancom) 5. März 2016
Petition calls on court to reverse decision on Zaman, urges Erdo�an to end crackdown on free press https://t.co/OSIWgeu9SJ
— Index on Censorship (@IndexCensorship) 5. März 2016
A Reading List for Future Journalistshttps://t.co/yqv9EPHWxc Via Columbia Journalism Review pic.twitter.com/pvEdo9vtM8
— Lotte Leicht (@LotteLeicht1) 5. März 2016
On International Women’s Day join PEN and Take Action for courageous women writers: https://t.co/bNJJl7OSLY #IWD2016 pic.twitter.com/QNCSBmQhoG
— PEN International (@pen_int) 5. März 2016
US decries #Zaman takeover as latest „troubling“ action by #Turkey govt against free press. #EU silence is shameful. https://t.co/k5Khhe17Ua
— Lotte Leicht (@LotteLeicht1) 5. März 2016
Yes, it’s not ‚rocket science‘ but many #EU govs prefer fear-mongering & xenophobia over collective humane solutions https://t.co/jhBxHp54Nj
— Lotte Leicht (@LotteLeicht1) 5. März 2016
Soll EU-Flüchtlingsgipfel mit Türkei nach Pol.Sturm auf Redaktion v #Zaman abgesagt werden? Nein, aber MR ignorieren geht nicht #deMaiziere
— Thomas Mayer (@TomMayerEuropa) 5. März 2016
Offener Brief v Vorstand der IG Architektur an BK Faymann, Innenministerin Mikl-Leitner u Außenminister Kurz https://t.co/0C55V8l7ou
— cariklaus (@KlausSchwertner) 5. März 2016
Stop fear-mongering: #Refugees are not mere numbers, they are ppl whose normal existence has been wrenched from them pic.twitter.com/TdxkabFgGN
— Lotte Leicht (@LotteLeicht1) 5. März 2016
To stigmatize #refugees as a threat or to insinuate that the flows are illegal and economic is harmful & plain wrong pic.twitter.com/9yDxydr0HU
— Lotte Leicht (@LotteLeicht1) 5. März 2016
#Zaman takeover is latest #Turkey move to crush independent media&scrutiny of govt policies https://t.co/7YhMuUTv3N pic.twitter.com/TnYSrR5U9P
— Lotte Leicht (@LotteLeicht1) 5. März 2016
Watch as police fire tear gas, use water cannon on hundreds of readers in front of #Zaman https://t.co/MGuncKEKDq pic.twitter.com/Rxl1skDX7W
— Today’s Zaman (@todayszamancom) 4. März 2016
Another blow to free speech in #Turkey: #Zaman takeover is nothing but a veiled move to eradicate opposition media pic.twitter.com/fJM0QZ4EJc
— Lotte Leicht (@LotteLeicht1) 5. März 2016
#Syria artist Nizar Ali Badr tells the #refugees‚ story using pebbles https://t.co/47w8iIzEhQ pic.twitter.com/GrHxj09290
— Lotte Leicht (@LotteLeicht1) 5. März 2016
An entire generation that never experienced anything other than life as a refugee pic.twitter.com/PEocOfQa4D https://t.co/9C6rEMLQ0h
— Alex Court (@CourtA) 1. Februar 2016
‚Constitution suspended‘ reads the headline of final edition of Zaman before violent takeover last night pic.twitter.com/jOlGz0QrzW
— Emma Sinclair-Webb (@esinclairwebb) 5. März 2016
Unglaublicher Satz. https://t.co/DZod3uUBqB
— Stefan Kappacher (@KappacherS) 5. März 2016
Europa im Jahr 2016#idomeni https://t.co/Eb6lrUaIFw
— cariklaus (@KlausSchwertner) 5. März 2016
Redakteure von @todayszamancom protestieren gegen die Stürmung ihrer Redaktion #Türkei #freepresscannotbesilenced https://t.co/2JD4wuSSyP
— ZDF heute (@ZDFheute) 5. März 2016
#Idomeni, Greece: War in Syria is putting a heavy burden on kids like Masoom. Couldn’t continue. We stopped to help pic.twitter.com/edIk0MXiPt
— Babar Baloch (@BabarBloch) 4. März 2016
Beim Sturm d türkischen Regierung gg kritische Journalisten zeigt sich, wie extrem heikel die Kooperation zu #refugees ist.
— Thomas Mayer (@TomMayerEuropa) 4. März 2016
If only nature would find a way to cover these oranges so we didn’t need to waste so much plastic on them. pic.twitter.com/00YECaHB4D
— Nathalie Gordon (@awlilnatty) 3. März 2016
Yet another black day for media freedom in #Turkey : Front page of @todayszamancom for Saturday pic.twitter.com/22OaSSdXk4
— Today’s Zaman (@todayszamancom) 4. März 2016
Prominent journalists, press groups show solidarity with #Zaman over takeover by gov’t https://t.co/TyLjBhc5MA pic.twitter.com/OD6dpgmZlm
— Today’s Zaman (@todayszamancom) 4. März 2016
Today’s Zaman chief editor posts „probably last message“ from her office after police raid https://t.co/NZI7xoz5al pic.twitter.com/jLF1EtKgls
— Today’s Zaman (@todayszamancom) 4. März 2016
#Greece: situation is quickly deteriorating with over 30,000 people at border https://t.co/2QdjsUGoKb pic.twitter.com/jQxAFfo1yF
— UN Refugee Agency (@Refugees) 5. März 2016
#Zaman takeover is latest blow to free speech in #Turkey & nothing but a veiled move to eradicate opposition media https://t.co/UCu5UfMa0O
— Lotte Leicht (@LotteLeicht1) 5. März 2016
Langes, gutes Interview mit Gerald Knaus über Merkels #Flüchtlingspolitik. Hinterfragen statt polemisieren https://t.co/tbjgUvG2UC
— Birgit Schmeitzner (@BSchmeitzner) 5. März 2016
#freepresscannotbesilenced https://t.co/BslZdqoqRz
— Birgit Schmeitzner (@BSchmeitzner) 5. März 2016