TCM – TRADITIONAL CHINESE MEDICINE
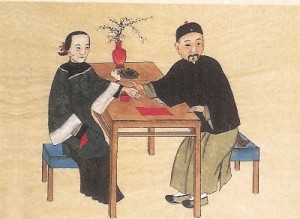
(Traditional Chinese Pulsediagnosis)
> ÖAGTCM: Österr. Ausbildung für TCM <
Traditional Chinese Medicine, also known as TCM, includes a range of traditional medicine practices originating in China. Although well accepted in the mainstream of medical care throughout East Asia, it is considered an alternative medical system in much of the Western world. TCM practices include such treatments as Chinese herbal medicine, acupuncture, dietary therapy, and both Tui na and Shiatsu massage. Qigong and Taijiquan are also closely associated with TCM.
Much of the philosophy of traditional Chinese medicine derives from the same philosophy that informs Taoist and Buddhist thought, and reflects the classical Chinese belief that the life and activity of individual human beings have an intimate relationship with the environment on all levels. Read More: > HERE <
TRADITIONAL CHINESE MEDICINE – Introduction – Traditional Chinese medicine (Simplified: ä��医学; Traditional: ä��醫學; Pinyin: zhōngyÄ� xué) is the name commonly given to a range of traditional medical practices used in China that have developed over the course of several thousand years of history. It is one of the most important forms of Oriental medicine, a term which may also include other related traditional Asian medical systems such as Japanese, Korean, Tibetan, and Mongolian medicine. Chinese medicine principally employs a method of analysis and synthesis, inquiring on a macro-level into the internal systems of the human body and their mutual relationships with the internal and external environment in an attempt to gain an understanding of the fundamental laws which govern the functioning of the human organism, and to apply this understanding to the treatment and prevention of disease, and health maintenance. TCM is rooted in a unique, comprehensive and systematic theoretical structure which includes the Theory of Yin-yang , the Five Elements, the human body Meridian system, and other systems. Treatment is conducted with reference to this philosophical framework.
Uses – In the West, TCM is often considered alternative medicine; however, in mainland China and Taiwan, TCM is widely considered to be an integral part of the health care system. The term TCM is sometimes used specifically within the field of Chinese medicine to refer to the standardized set of theories and practices introduced in the mid-20th century under the government of Mao, as distinguished from related traditional theories and practices preserved by people in Taiwan, Hong Kong and by the overseas Chinese. The more general sense is meant in this section.
TCM developed as a form of noninvasive therapeutic intervention (also described as folk medicine or traditional medicine) rooted in ancient belief systems, including traditional religious concepts. Chinese medical practitioners before the 19th century relied on observation, trial and error, which incorporated certain mystical concepts. Like their Western counterparts, doctors of TCM had a limited understanding of infection, which predated the discovery of bacteria, viruses (germ theory of disease) and an understanding of cellular structures and organic chemistry. Instead they relied mainly on observation and description on the nature of infections for creating remedies. Based on theories formulated through three millennia of observation and practical experience, a system of procedure was formed as to guide a TCM practitioner in courses of treatment and diagnosis.
Unlike other forms of traditional medicine which have largely become extinct, traditional Chinese medicine continues as a distinct branch of modern medical practice, and within China, it is an important part of the public health care system. There are thousands of years of empirical knowledge about TCM conceptualized and recorded in terms appropriate to that system, and in recent decades there has been an effort to integrate the discoveries made by traditional Chinese medicine with the discoveries made by workers in the Western medical traditions. One important component of this work is to use the instrumentation and the methodological tools available via Western medicine to investigate observations made and hypotheses raised by the Chinese tradition.
That this effort has occurred is surprising to many for a number of reasons. In most of the world, indigenous medical practices have been supplanted by practices brought from the West, while in Chinese societies, this has not occurred and shows no sign of occurring. Furthermore, many have found it peculiar that Chinese medicine remains a distinct branch of medicine separate from Western medicine, while the same has not happened with other intellectual fields. There is, for example, no longer a distinct branch of Chinese physics or Chinese biology.
TCM is used by some to treat the side effects of chemotherapy, treating the cravings and withdrawal symptoms of drug addicts and treating a variety of chronic conditions that conventional medicine is claimed to be sometimes ineffective in treating. TCM has also been used to treat antibiotic-resistant infection.
A report issued by the Victorian state government in Australia describes TCM education in China: – Graduates from TCM university courses are able to diagnose in western medical terms, prescribe western pharmaceuticals, and undertake minor surgical procedures. In effect, they practice TCM as a specialty within the broader organization of Chinese health care.
TCM education in Australia, however, does not qualify a TCM practitioner to prescribe scheduled pharmaceuticals, nor to undertake surgical procedures or diagnose in western medical terms.
Theory – There are many schools of thought on which TCM is based. Because of this, the foundation principles of Chinese medicine are not necessarily uniform. Received TCM can be shown to be most influenced by Taoism, Buddhism, and Neo-Confucianism.
For over 3000 years (1200 BCE- present), Chinese academics of various schools have focused on the observable natural laws of the universe and their implications for the practical characterization of humanity’s place in the universe. In the I Ching and other Chinese literary and philosophical classics, they have described some general principles and their applications to health and healing:
- There are observable principles of constant phenomenal change by which the Universe is maintained.
- Man is part of the universe and cannot be separated from the universal process of change.
- As a result of these apparently inescapable primordial principles, the Universe (and every process therein) tends to eventually balance itself.
- Optimum health should result from living as harmoniously as possible with the spontaneous process of change tending towards balance. If there is no change (stagnation), or too much change (catastrophism), balance is increasingly lost and illnesses can occur.
- Everything is ultimately interconnected.
- Always use a systemic approach when addressing imbalances.
TCM is therefore largely based on the philosophical concept that the human body is a small universe with a set of complete and sophisticated interconnected systems. Those systems usually work in balance to maintain the healthy function of the human body. The balance is described as necessarily including qi, blood, jing, bodily fluids, the wu xing, emotions, and spirit (shen). TCM has a unique model of the body, notably concerned with the meridian system. TCM isn’t monolithic, however, and there are from minor to significant regional and philosophical differences between practitioners and schools which in turn can lead to differences in practice and theory.
Macro Views to Diseases – TCM has a macro view to most diseases: well-balanced human bodies can usually handle most everyday bacteria and virus, which are ubiquitous and fastly changing; diseases happens only if there are some unbalanced parts in a human body. Due to this macro philosophy, TCM usually does not care what exact bacteria or virus are causing the symptoms, but tries the best to find which parts of the body are unbalanced as well as to find a strategy to bring back the balance. At the meantime, TCM believes only symptoms matter because irregular symptoms from the human bodies are the only faithful sources to deduce the unbalanced parts in a dynamic, complex system like a human body.
Consequently, the treatments in TCM do not directly target to kill bacteria or virus but to bring back the balance of human bodis. It is very surprising but understandable that a TCM doctor may give very different herb prescriptions to patients affected by a same type of bacteria, because the different symptoms from the patients indicate different unbalanced parts in their bodies.
TCM’s macro view to diseases has some advantages and limitations compared to modern western medicine, which directly targets the external factors of diseases like bacteria and virus.
* The biggest advantage of TCM is that the internal reasons of diseases are addressed and the details of bacteria and virus can be largely ignored. The real potentials of the well-evolved human bodies are used to fight the bacteria and virus instead of simple antibiotics.
A correct TCM treatment will not only address current disease but also establish a strong balance to fight any other diseases. This is especially useful when the abused antibiotics fasten the mutation of bacteria and virus nowadays and it is increasingly difficult for doctors to develop right drugs to kill some specific variants. More over, the downside of western drugs is that they kill not only the bad bacteria and virus but they also severely intervene in the proper functioning of human bodies, which in turn worsen the unbalanced human internal system and make patients more susceptible to other types of bacteria and virus. This is the biggest dilemma in modern western medicine as exemplify by chemotherapy and radiotherapy treatments to cancers.
* A TCM doctor handles many types of diseases from hearts, livers, lungs, etc because the macro view of human body. A patient can be helped by just one visit to a TCM doctor in a comprehensive way. On the other hand, modern western medicine adopts a micro view. The diagnoses and treatments to diseases are highly specialized in terms of different causes. Patients have to judge first which specialist is going to help their problems.
* Judging the effectiveness of treatments in TCM is also based on a macro point of view. Genuine TCM does not rely on micro level lab test results like blood pressure, liver function, a report, bacteria numbers etc. Instead, macro level human feelings and behaviors are used: such as the sleep quality, feeling of enough energy to handle daily work, appetite to food, normal excreting, warmness of hands and feet etc. Modern western medicine relies on the lab tests to see the effectiveness of a treatment using drugs: like how many bacteria are left in the body. TCM doctors often criticize that western doctors pays too much attentions to individual metrics in lab reports and less concerns are given to the overall feelings of patients.
* The cost associated with TCM diagnoses and treatments are usually much less than modern western ways, which requires high-tech equipments and lab facilities to locate the external details. It is relatively fair for both the rich and the poor when seeing a TCM doctor and using Chinese herbs.
* The major problem in TCM is that a right disease diagnosis highly depends on the experiences of a TCM doctor. Even with a right diagnosis, a proper strategy using combined herb prescriptions must be used to bring back the dynamic balance in human bodies. As a result, it takes years or even decades to train a good TCM doctor who can deduce the unbalanced parts from complex symptoms from patients and find a right solution for it considering the interconnection between different parts in human bodies. There is a Chinese saying describing the wisdom and experiences needed for a TCM doctor: A good TCM doctor is also qualified to be a good prime minister in a country. In contrast, modern western diagnoses and treatments are more reliable than TCM in the sense that clear procedures are defined and the accurate information of bacteria and virus can be obtained.
* Finally, TCM may fail if a patient’s internal balance has been ruined too much and immediate, direct solution must be used to fight the diseases. TCM just does not know what bacteria and virus are the culprits.
It is natural for people to think a combined way to fight diseases from both internal and external point of views. Many doctors are researching into this promising areas.
Diagnostics – Following the macro philosophy, TCM diagnostics are based on overall observation of human syptoms rather than micro level labs. There are four types of TCM diagnostic methods: observe (望 wàng), hear and smell (聞 wén), ask about background (問 wèn) and read the pulse (切 qiè). Then a diagnosis is made using a system to classify the symptoms. As mentioned earlier, diagnostic based on symptoms, not bacteria or virus, is the essence in TCM because the internal reasons in human bodies matter.
Systems of diagnosis include:
- * Yin or Yang
- * Five Elements
- * Eight Principles
- * Zang Fu theory
- * Meridian (Chinese medicine)
- * Six Levels
- * Four Stages
- * Three Jiao
TCM diagnosis in China is becoming integrated with western diagnostic thought and is moving towards total integration of the two systems. Modern practitioners in China often use the two systems in combination to understand what is happening with the patient.
Because traditional Chinese medicine predates the more invasive medical testing used in conventional Western medicine, TCM requires skill in a range of diagnostic systems not commonly used outside of TCM. Much of this diagnostic skill involves developing the abilities to observe subtle appearances; to observe that which is right in front of us, but escapes the observation of most people. SEE Also: Traditional Chinese Medicine :: Diagnostic Theory
Diagnostic Techniques
- Palpation of the patient’s radial artery pulse in six positions
- Observation of the appearance of the patient’s tongue
- Observation of the patient’s face
- Palpation of the patient’s body (especially the abdomen) for tenderness
- Observation of the sound of the patient’s voice
- Observation of the surface of the ear
- Observation of the vein on the index finger on small children
- Comparisons of the relative warmth or coolness of different parts of the body
- Anything else that can be observed without instruments and without harming the patient
- SEE Also: Traditional Chinese Medicine :: Diagnostic Theory
Treatment Techniques
- Historically, eight branches comprised Chinese medicine treatment:
- Tui na(推拿) Chinese Massage Therapy
- Acupuncture and Moxibustion(針灸)
- Chinese herbal medicine(ä��药)
- Chinese food therapy食 疗
- Qigong(氣功) and related breathing and meditation exercise
- T’ai Chi Ch’uan (太極拳) and other Chinese martial arts.
- Feng shui风水
- Chinese astrology
Today, all methods except Feng shui and Chinese astrology are routinely used as part of TCM treatments.
Within each treatment branch, specific treatment methods exist. Cupping and Gua sha(刮痧) come under the heading of Tui Na. Auriculotherapy(耳燭療法) comes under the heading of Acupuncture and Moxibustion. Die-da or Tieh Ta (跌打): practitioners who specialize in healing trauma injury such as bone fractures, sprains, bruises etc. Some of these specialists may also use or recommend other disciplines of Chinese medical therapies (or Western medicine in modern times) if serious injury is involved. Such practice of bone-setting is not common in the West.
Modern TCM treatments consist of herbal medicine or acupuncture as the primary method, with other methods such as massage, qi gong, food therapy playing a secondary role. Illness in TCM is seen as a lack of harmony, and the goal of all TCM treatment is to assist the body to regain balance and achieve homeostasis.
The modern practice of traditional Chinese medicine is increasingly incorporating techniques and theories of Western medicine in its praxis.
SEE Also:
- * Health :: Acupuncture
- * Traditional Chinese Medicine :: Moxibustion
- * Traditional Chinese Medicine :: Qigong
- * Traditional Chinese Medicine :: Herbology
- * Traditional Chinese Medicine :: Food Therapy
Traditional Chinese Medicine and Science, The Question of Efficacy – Most scientific research about TCM has focused on acupuncture. Two views have emerged characterized by evidence based medicine on the one hand which has not found convincing evidence for acupuncture and the United States National Institutes of Health on the other, which believed evidence could be uncovered. The 1997 NIH Consensus Statement on Acupuncture summarizes research on the efficacy of acupuncture as follows:
„…promising results have emerged, for example, efficacy of acupuncture in adult post-operative and chemotherapy nausea and vomiting and in postoperative dental pain. There are other situations such as addiction, stroke rehabilitation, headache, menstrual cramps, tennis elbow, fibromyalgia, myofascial pain, osteoarthritis, low back pain, carpal tunnel syndrome, and asthma for which acupuncture may be useful as an adjunct treatment or an acceptable alternative or be included in a comprehensive management program. Further research is likely to uncover additional areas where acupuncture interventions will be useful.“
Much less work in the West has been done on Chinese herbal medicines, which comprise much of TCM. It is clear, however, that some of these medicines have powerful biochemical effects. An example is the herb ephedra which was introduced into the West as a stimulant, and later banned (although this ban was ordered lifted in 2005 by a federal court judge) in the United States after deaths were attributed to its use. A less controversial example is artemisinin, derived from a herb long-used used in TCM, and now used worldwide to treat multi-drug resistant strains of falciparum malaria. In the West, many Chinese medicines have been marketed as herbal supplements and there has been considerable controversy over the regulatory status of these substances.
TCM practitioners usually have no philosophical objections to scientific studies on the effectiveness of treatments. A barrier to the adoption of Chinese herbal medicines into Western practice is finance. It requires a large amount of expertise and money to conduct, for example, a double-blind drug trial, making it a large venture to test even one of the thousands of compounds used by TCM. Because these compounds cannot be patented and owned exclusively, there is a disincentive to sponsor such expensive tests. Some important western medical drugs such as Ephedrine have come from Chinese herbs.
There are also a priori doubts about the efficacy of many TCM treatments that appear to have their basis in magical thinking, e.g. plants with heart-shaped leaves will help the heart, ground bones of tiger give a person energy because tigers are energetic animals and so on.
Purported Mechanism of Action – The basic mechanism of TCM is akin to treating the body as a black box, recording and classifying changes and observations of the patient using a traditional philosophy. In contrast to many alternative and complementary medicines such as homeopathy, practically all techniques of TCM have explanations for why they may be more effective than a placebo, which Western medicine can find plausible. Most doctors of Western medicine would not find implausible claims that qigong preserves health by encouraging relaxation and movement, that acupuncture relieves pain by stimulating the production of neurotransmitters, or that Chinese herbal medicines may contain powerful biochemical agents. However, the largest barriers to describing the mechanisms of TCM in scientific terms are the difference of language and lack of research. TCM concepts such as qi yin and yang are used to describe specific biological processes but are difficult to translate into scientific terms. Some research is now beginning to emerge explaining possible scientific mechanisms behind these TCM concepts.
Safety of Chinese Medicines – Acupressure and acupuncture are largely accepted to be safe from results gained through medical studies. Several cases of pneumothorax, nerve damage and infection have been reported as resulting from acupuncture treatments. These adverse events are extremely rare and were found to be due to practitioner negligence. Dizziness and bruising will sometimes result from acupuncture treatment.
Chinese herbal medicines, in certain cases, involve risk of poisoning or allergic reactions. Cases of acute and chronic poisoning due to treatment through ingested Chinese medicines are relatively common in China, Hong Kong, and Taiwan, with numerous deaths occurring each year. Many of these deaths do occur however, when patients self prescribe herbs or take unprocessed versions of toxic herbs. For example, the Chinese herb má huáng — known commonly in the west by its Latin name Ephedra — was banned in 2004 by the FDA, although, the FDA’s final ruling exempted traditional Asian preparations of Ephedra from the ban. The Ephedra ban was meant to combat the use of this herb in western weight loss products, a usage that directly conflicts with traditional Asian uses of the herb. There were no cases of Ephedra based fatalities with patients using traditional Asian preparations of the herb for its traditionally intended uses. This ban was ordered lifted in April 2005 by a Utah federal court judge.
Furthermore, potentially toxic and carcinogenic compounds such as arsenic and cinnabar are sometimes prescribed as part of a medicinal mixture or used on the basis of „using poison to cure poison“. Unprocessed herbals are sometimes adulterated with chemicals that may alter the intended effect of a herbal preparation or prescription. Much of these are being prevented with more empirical studies of Chinese herbals and tighter regulation regarding the growing, processing, and prescription of various herbals.
Traditional Chinese Medicine and Western Medicine – Within China, there has been a great deal of cooperation between TCM practitioners and Western medicine, especially in the field of ethnomedicine. Chinese herbal medicine includes many compounds which are unused by Western medicine, and there is great interest in those compounds as well as the theories which TCM practitioners use to determine which compound to prescribe. For their part, advanced TCM practitioners in China are interested in statistical and experimental techniques which can better distinguish medicines that work from those that do not. One result of this collaboration has been the creation of peer reviewed scientific journals and medical databases on traditional Chinese medicine.
The relationship between TCM and Western medicine in the West is more contentious. While more and more medical schools are including classes on alternative medicine in their curricula, older Western doctors and scientists are far more likely than their Chinese counterparts to skeptically view TCM as archaic pseudoscience and superstition. This skepticism can come from a number of sources. For one, TCM in the West tends to be advocated either by Chinese immigrants or by those that have lost faith in conventional medicine. Many people in the West have a stereotype of the East as mystical and unscientific, which attracts those in the West who have lost hope in science and repels those who believe in scientific explanations. There have also been experiences in the West with unscrupulous or well-meaning but improperly-trained „TCM practitioners“ who have done people more harm than good in many instances.
As an example of the different roles of TCM in China and the West, a person with a broken bone in the West (i.e. a routine, „straightforward“ condition) would almost never see a Chinese medicine practitioner or visit a martial arts school to get the bone set, whereas this is routine in China. As another example, most TCM hospitals in China have electron microscopes and many TCM practitioners know how to use one.
This is not to say that TCM techniques are considered worthless in the West. In fact, Western pharmaceutical companies have recognized the value of traditional medicines and are employing teams of scientists in many parts of the world to gather knowledge from traditional healers and medical practitioners. After all, the active ingredients of most modern medicines were discovered in plants or animals. The particular contribution of Western medicine is that it strictly applies the scientific method to promising traditional treatments, separating those that work from those that do not. As another example, most Western hospitals and increasing numbers of other clinics now offer T’ai Chi Ch’uan or qigong classes as part of their inpatient and community health programs.
Most Chinese in China do not see traditional Chinese medicine and Western medicine as being in conflict. In cases of emergency and crisis situations, there is generally no reluctance in using conventional Western medicine. At the same time, belief in Chinese medicine remains strong in the area of maintaining health. To put it simply, you see a Western doctor if you have acute appendicitis, but you do exercises or take Chinese herbs to keep your body healthy enough to prevent appendicitis, or to recover more quickly from the surgery. Very few practitioners of Western medicine in China reject traditional Chinese medicine, and most doctors in China will use some elements of Chinese medicine in their own practice.
A degree of integration between Chinese and Western medicine also exists in China. For instance, at the Shanghai cancer hospital, a patient may be seen by a multidisciplinary team and be treated concurrently with radiation surgery, Western drugs and a traditional herbal formula.
It is worth noting that the practice of Western medicine in China is somewhat different from that in the West. In contrast to the West, there are relatively few allied health professionals to perform routine medical procedures or to undertake procedures such as massage or physical therapy.
In addition, Chinese practitioners of Western medicine have been less impacted by trends in the West that encourage patient empowerment, to see the patient as an individual rather than a collection of parts, and to do nothing when medically appropriate. Chinese practitioners of Western medicine have been widely criticized for overprescribing drugs such as corticosteroids or antibiotics for common viral infections. It is likely that these medicines, which are generally known to be useless against viral infections, would provide less relief to the patient than traditional Chinese herbal remedies.
Traditional Chinese Medicine and Animals – As animal products are used in Chinese formulas, vegans and vegetarians should inform their practitioner, if their beliefs forbid the ingestion of animals. Often alternative substances can be used.
The use of endangered species is controversial within TCM. In particular, the belief that tiger penis and rhinoceros horn are aphrodisiacs has been blamed for depleting these species in the wild. Medicinal use is also having a major impact on the populations of sea horses.
The animal rights movement notes that a few traditional Chinese medicinal solutions use bear bile. To extract maximum amounts of the bile, the bears are often fitted with a sort of permanent catheter. The treatment itself and especially the extraction of the bile is very painful, causes damage to the intestines of the bear, and often even kills the bears. However, due to international attention on the issues surrounding its harvesting, bile is now rarely used by practitioners outside of China.
- Sources
- * Chang, Stephen T. The Great Tao; Tao Longevity; ISBN 0942196015 Stephen T. Chang
- * Kaptchuck, Ted J., The Web That Has No Weaver; Congdon & Weed; ISBN 0809229331Z
- * Maciocia, Giovanni, The Foundations of Chinese Medicine: A Comprehensive Text for Acupuncturists and Herbalists; Churchill Livingstone; ISBN 0443-039801
- * Ni, Mao-Shing, The Yellow Emperor’s Classic of Medicine : A New Translation of the Neijing Suwen with Commentary; Shambhala, 1995; ISBN 1570620806
- * Holland, Alex Voices of Qi: An Introductory Guide to Traditional Chinese Medicine; North Atlantic Books, 2000; ISBN 1556433263
- * Unschuld, Paul U., Medicine in China: A History of Ideas; University of California Press, 1985; ISBN 0520050231
- * Qu, Jiecheng, When Chinese Medicine Meets Western Medicine – History and Ideas (in Chinese); Joint Publishing (H.K.), 2004; ISBN 9620423364
- * Chan, T.Y. (2002). Incidence of herb-induced aconitine poisoning in Hong Kong: impact of publicity measures to promote awareness among the herbalists and the public. Drug Saf. 25:823–828.
- * Benowitz, Neal L. (2000) Review of adverse reaction reports involving ephedrine-containing herbal products. Submitted to U.S. Food and Drug Administration. Jan. 17.
- * Porkert, Manfred The Theoretical Foundations of Chinese Medicine MIT Press, 1974 ISBN 0262160587
- * Hongyi, L., Hua, T., Jiming, H., Lianxin, C., Nai, L., Weiya, X., Wentao, M. (2003) Perivascular Space: Possible anatomical substrate for the meridian. Journal of Complimentary and Alternative Medicine. 9:6 (2003) pp851-859
Links
- State Administration of Traditional Chinese Medicine for the People’s Republic of China, (English)
- Journal of Chinese Medicine
- Classics of Traditional Chinese Medicine, by the National Library of Medicine (NLM)
- Merging Chinese Traditional Medicine into the American Health System
- The Chinese Medicine Sampler- Historical Roots of Traditional Chinese Medicine
- An essay on translation of Chinese concepts into English
- Traditional Chinese Medicine news, information, education, research and discussion – A regularly updated TCM website based in Australia
- ChineseMedicine.com.hk 香港ä��醫網
- National Certification Commission for Acupuncture and Oriental Medicine (USA)
- University Minnesota – What is TCM ?
- AHC – Center for Spirituality and Healing
- QI GONG im Kloster St. Clemens, July 2010
- Guang’anmen HOSPITAL, CHINA ACADEMY of Chinese Medical Sciences
- Meet QI-GONG Groups and Friends at facebook <
Comments are closed.